Amy Medling's Blog
August 27, 2025
215 – Healing hormonal acne from the inside – The gut connection
Dr. Barbara Paldus is the founder of Codex Labs. Codex Labs is a holistic acne management strategy, covering everything from cleansers, spot treatments and supplements. Dr. Paldus explains the powerful connection between gut health, inflammation, and chronic skin issues like adult female hormonal acne, eczema, and teen acne.
Tune in as they discuss:
Processed foods effects on acneHow many days it takes to reset your gutHow plants have co evolved with humansHidden dangers of overusing antibiotics and its impact on gut healthSkincare and nutritionResources Mentioned:Codex WebsiteCodex Labs Instagram
Canadian-born of Czech parents and fluent in five languages with a Ph.D. from Stanford University (U.S.), Dr. Barbara Paldus holds over 50 US patents and is a serial entrepreneur, having started companies like Picarro (greenhouse gas detection for climate change) and Finesse Solutions (biotechnology equipment for vaccines like COVID-19, cancer therapeutics and cell therapy).
Codex Labs was conceived with dermatologists and ethnobotanists to deliver affordable, clinically proven skin-gut-brain solutions that support the microbiome and delivery healthy skin, without sacrificing sustainability.
July 16, 2025
215- Healing Hormonal acne from the inside – The gut connection [Podcast with Dr. Barbara Paldus]
Dr. Barbara Paldus explains the powerful connection between gut health, inflammation, and chronic skin issues like adult female hormonal acne, eczema, and teen acne.
Dr. Barbara Paldus is the founder of Codex Labs. Codex Labs is a holistic acne management strategy, covering everything from cleansers, spot treatments and supplements.
Tune in as they discuss:Skincare and nutritionProcessed foods effects on acneHow many days it takes to reset your gutHow plants have co evolved with humansHidden dangers of overusing antibiotics and its impact on gut healthpcosdiva · 215- [Podcast with Dr. Barbara Paldus] Healing Hormonal acne from the inside – The gut connectionpcosdiva · 215- [Podcast with Dr. Barbara Paldus] Healing Hormonal acne from the inside – The gut connectionResources Mentioned:Codex Labs Instagram

Dr. Barbara Paldus is a Canadian-born of Czech parents and fluent in five languages with a Ph.D. from Stanford University (U.S.), Dr. Barbara Paldus holds over 50 US patents and is a serial entrepreneur, having started companies like Picarro (greenhouse gas detection for climate change) and Finesse Solutions (biotechnology equipment for vaccines like COVID-19, cancer therapeutics and cell therapy).
Codex Labs was conceived with dermatologists and ethnobotanists to deliver affordable, clinically proven skin-gut-brain solutions that support the microbiome and delivery healthy skin, without sacrificing sustainability.
The post 215- Healing Hormonal acne from the inside – The gut connection [Podcast with Dr. Barbara Paldus] appeared first on PCOS Diva.
June 26, 2025
New Technology – Getting Fertility Answers Faster
[image error]Women with Polycystic Ovarian Syndrome (PCOS) know what a challenge it can be to get a formal diagnosis. Unfortunately, many of us have experienced it ourselves. Often, weight gain, acne, hirsutism, and irregularity are not taken seriously until that results in infertility, and many of us only get to this point years or even decades after our symptoms began.
One in eight couples will have trouble getting pregnant or carrying a baby to term, however many are left frustrated without a formal diagnosis to explain their challenges. While some causes are truly unknown, others go undiagnosed as there is not enough information available or the signs go undetected. This is particularly true in cases involving PCOS. Our cycle patterns rarely conform to the “norm.” Ovulation prediction kits and fertility monitors are often useless.
I have written about OvuSense before and how it can be a game-changer helping women with PCOS gain awareness of their cycles and get pregnant, but recently the company has developed a new technology to help women with conditions like PCOS make the most of their data, called OvuSense Pro. For years women have been using the information from OvuSense’s Core Body Temperature (CBT) monitoring technology to help them get pregnant, but now women and their doctors actually use the same data to identify otherwise undetectable causes of infertility, in the hopes of addressing and tailoring their care sooner.[image error]
Using data to find answers, rather than “wait and see”For those who may not be familiar with OvuSense, it is the only FDA approved Class 2 fertility monitor designed to help understand the link between cycle characteristics of CBT curves and infertility. In recent research, presented at the 2019 American Society for Reproductive Medicine (ASRM) meeting, the OvuSense team assessed a range of “atypical cycle patterns” common in women with ovulatory conditions such as PCOS, within the OvuSense user base.
In a recent article, Fertility Focus CEO Rob Milnes explained how the new research aims to help women and their doctors uncover previously unidentified fertility issues without having to simply “wait and see” and struggle before getting a diagnosis. Knowing this information in advance may help doctors diagnose ovulatory issues and then monitor treatment, helping to remove some of the doubt around “unexplained” infertility, enable timely intervention or prevent recurrent miscarriages.
No Such Thing as Typical PCOS Cycle“…a significant number of women with ovulatory issues never receive a satisfactory diagnosis. The ability of women over the age of 30 to conceive naturally within a year declines by around 5% per year, so with the demographic shift, it is now essential to find out if there is an ovulatory issue as soon as possible.”
Essentially what the OvuSense study found — and what many women with PCOS already know— is that there is no such thing as a typical cycle pattern. However, when you look at the data and experiences of thousands of women, there are some patterns that while often go unrecognized can be indicative of certain conditions that greatly impact our fertility.
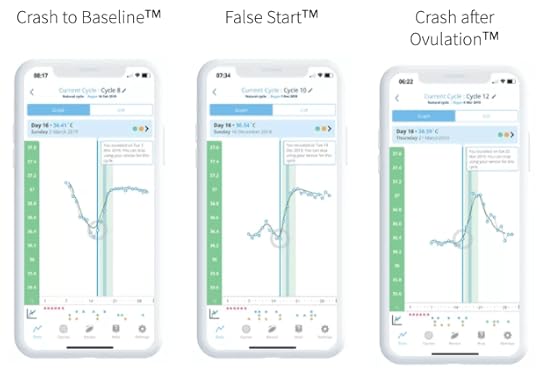
Using Technology to Identify 3 New Cycle PatternsOne of those patterns called ‘‘Crash to Baseline’’ suggests high progesterone early in the cycle. Another, called ‘‘False Start’’ suggests an initial surge in luteinizing hormone with an accompanying small progesterone rise. Both of these abnormal temperature patterns would be expected to occur in women with PCOS, and the study investigators do indeed plan to test this hypothesis. ‘‘Crash After Ovulation” suggests that progesterone may fall sharply in some women before the onset of their period, and it is possible that fertility may be impaired in these cycles.
 What OvuSense hopes this research and the release of OvuSense Pro boils down to, is that they want to help women before they have problems conceiving — to not only help them start their families when they choose, but also provide valuable information about their health.
What OvuSense hopes this research and the release of OvuSense Pro boils down to, is that they want to help women before they have problems conceiving — to not only help them start their families when they choose, but also provide valuable information about their health.
Particularly if you’ve had trouble trying to get pregnant or even fighting to get diagnosed for PCOS, working with a doctor is an important part of your journey. However, this isn’t always a 24/7 line of information. By using tools like OvuSense at home, you can begin to recognize patterns in your cycle in between appointments, making your in-person visits with your physician more productive since you’re armed with more information about your cycle.
The new platform allows an OvuSense user and their doctor to access detailed cycle information through an online portal. It provides unique key analysis about cycle patterns to help medical professionals to know whether they need to carry out further tests, what effect medications are having, to time tests like blood progesterone and ultrasound, to understand what’s happening during treatment, and to understand whether medications, treatment or dietary change are having an effect on the timing of ovulation and the length of cycles.
Some of these cycle patterns include those that were presented at ASRM last year, but it has also expanded to indicate early ovulation, late ovulation, anovulation, short luteal phase, and more. By easily pinpointing these cycle characteristics within your cycle, you and your physician can more quickly identify which hormones may be out of balance or identify changes or supplements that can support different elements of your fertility.

May 22, 2025
214 – Effective strategies for weight loss and balancing blood sugar-[Podcast with Nagina Sethi Abdullah]

My name is Nagina Abdullah and I’m a weight loss coach and the founder of Masala Body.
As an online weight loss coach, I’ve used my methodology to help female professionals and corporate executives achieve their dream weight and bodies even if they work 60+-hour weeks. I work directly with professional women to help them look amazing in everything they wear.
The post 214 – Effective strategies for weight loss and balancing blood sugar-[Podcast with Nagina Sethi Abdullah] appeared first on PCOS Diva.
May 1, 2025
213- How to break the cycle of emotional eating and find balance with food [Podcast with Elizabeth Dall]
Elizabeth Dall is a certified women’s nutrition coach, food freedom expert, and behavior change coach who specializes in helping women like break free from the diet cycle, make peace with food, and create sustainable, healthy habits.
With a holistic approach rooted in mindset shifts, self-compassion, and practical strategies, Elizabeth helps women to stop overeating, embrace their bodies, and achieve their health goals without guilt, restriction, or dieting.
In this podcast episode Elizabeth explains how to make mindful eating choices and why that is the first step to making peace with food. She says “Every women has the gift on knowing when her body is full and meeting the needs of her body.”
Tune in as they discuss:How emotional eating is actually telling you somethingWhy mindful eating creates a peaceful balance with foodThe importance of putting screens away while eatingBenefits of using a guided meditation while eating to learn how to experience the foodElizabeth’s thoughts on fastingHow to break out of the diet cycle
pcosdiva · 213- [Elizabeth Dall] How to break the cycle of emotional eating and find balance with food
pcosdiva · 213- [Elizabeth Dall] How to break the cycle of emotional eating and find balance with food
Resources Mentioned:Elizabeth Dall Website A Women of WellnessFree mindful eating meditation: A Women of Wellness Instagram The Women of Wellness Podcast

Elizabeth Dall is a women’s wellness coach, certified nutrition coach, and exercise physiologist passionate about helping women make peace with food, embrace their bodies, and create sustainable habits for a vibrant, fulfilling life.
Elizabeth is the host of The Woman of Wellness Podcast, she shares expert insights, actionable tools, and inspiring stories to support you on your wellness journey. Her coaching programs and resources are designed to help women build consistency, overcome challenges, and create lasting change so they can feel confident, healthy, and free with their relationship with food and their body.
The post 213- How to break the cycle of emotional eating and find balance with food [Podcast with Elizabeth Dall] appeared first on PCOS Diva.
March 13, 2025
212- Traditional Chinese Medicine for Migraine Care [Podcast with Diane Ducarme]
Diane Ducarme is the Founder & CEO of Migraine Heroes, is a leading figure in migraine investigation, blending the wisdom of Eastern Medicine with Western science and advanced technology to uncover the true roots of migraine disease.
Diane’s approach uniquely emphasizes adding functional foods instead of eliminating them, shifting away from restrictive practices to focus on nourishing the body. Diane’s dedication continues to transform lives, offering a holistic path to relief, resilience, and wellness for those navigating migraine disease.
Dr. Vinu and Diane discuss how 1 in 5 women have migraines and how migraines triple to quadruples for women once they reach puberty. Diane explains how the migraine attacks possibly are started in the digestive and hormonal systems. They also discuss how your gut has such a profound impact on the health of your brain. A healthy, balanced gut means no more error messages. No more error messages means no more migraines.Tune in as they discuss:How migraines are geneticThe importance of a balanced gut for migrainesDiet modifications for migrainesWhy the birth control pill is over prescribed for migrainesHow to get rid of a migraine naturallypcosdiva · 212- Traditional Chinese Medicine for Migraine Care [Podcast with Diane Ducarme]pcosdiva · 212- Traditional Chinese Medicine for Migraine Care [Podcast with Diane Ducarme]Resources Mentioned:Diane Ducarme Website: https://www.mynectarhealth.com/Take The Free Test: https://nectarhealth.typeform.com/migraine-testMigraine Heroes Chat: https://migraineheroeschat.netlify.appMigraine Heroes Podcast: https://www.migraineheroes.orgMigraine Heroes App Link at Apple Store: https://apps.apple.com/app/id6446701680Migraine Heroes App Link at Google Play : https://play.google.com/store/apps/details?id=com.nectarhealth

Diane Ducarme, Founder & CEO of Migraine Heroes, is a leading figure in migraine investigation, blending the wisdom of Eastern Medicine with Western science and advanced technology to uncover the true roots of migraine disease. With an MBA from Harvard Business School, a background in science and engineering, and fluency in seven languages—including Mandarin—Diane brings a rich perspective to the complex world of migraine care. Her journey has taken her from engineering to Traditional Chinese Medicine studies in China and, more recently, neuroscience research at Harvard X.
The post 212- Traditional Chinese Medicine for Migraine Care [Podcast with Diane Ducarme] appeared first on PCOS Diva.
February 3, 2025
211 – Women’s health and fertility – what your cycle is telling you [Podcast with Dr. Monica Minjeur]
[image error]
Dr. Monica Minjeur, is a board-certified family medicine physician specializing in testing and treatment for infertility, endometriosis, PCOS, recurrent miscarriage, painful periods, PMS and other gynecological conditions. She is passionate about using menstrual cycle analysis to improve the lives of women and couples.
In this episode she shares her expertise on the fertility awareness method (FAM), the effects of birth control including an IUD, and insights into natural treatments for the root causes of PCOS. This is such a valuable episode to listen to if you want to learn more about how your menstrual cycle works for all the different stages of life and the benefits of really learning what’s going on with your body.
Tune in as they discuss:
How ovulation is vital to knowing what’s going on with your healthNatural treatments for the root cause of PCOSThe importance of insulin resistance testingIVF, what to know when exploring different clinicsFertility awareness based method – how to track your cycle to prevent pregnancyBenefits of an anti-inflammatory diet (free of dairy, gluten, and refined sugar)pcosdiva · 211 – Women’s health and fertility-what your cycle is telling you [Podcast with Dr. Monica Minjeur]pcosdiva · 211 – Women’s health and fertility-what your cycle is telling you [Podcast with Dr. Monica Minjeur]
pcosdiva · 211 – Women’s health and fertility-what your cycle is telling you [Podcast with Dr. Monica Minjeur]
Resources Mentioned:Radiant Clinic WebsitePodcastFree discovery call to talk directly to Dr. Monica Minjeur

Dr. Monica Minjeur, DO, is the founder and CEO of Radiant Clinic. She is a board-certified family medicine physician specializing in testing and treatment for infertility, endometriosis, PCOS, recurrent miscarriage, painful periods, PMS and other gynecological conditions. She is passionate about using menstrual cycle analysis to improve the lives of women and couples.
The post 211 – Women’s health and fertility – what your cycle is telling you [Podcast with Dr. Monica Minjeur] appeared first on PCOS Diva.
October 25, 2024
210 – Cheating your way to good health [Podcast with Dr. Dana Cohen]

We’re so happy to have Dr. Dana Cohen back on the PCOS Diva Podcast! This episode we’ll learn about Dana’s new book Fuel Up, Harness the Power of Your Blender and Cheat Your Way to Good Health.
Dr. Cohen explains how to boost your nutrition through a blender. She breaks down how blended up food does not make them lose nutrients and how smoothies have so many health benefits.
Tune in as they discuss:
Why cheating or hacking your diet is okayDoes blended up food lose nutrients?The Role of blending in nutritionHow to properly hydrateCheat your way into eating more vegetablespcosdiva · 210 – Cheating your way to good health [Podcast with Dr. Dana Cohen]
Resources Mentioned:
The Benefits of Proper Hydration [Podcast with Dr. Dana Cohen]

For over two decades, Dr. Dana Cohen has been on the leading edge of integrative and functional medicine, guiding thousands of patients through protocols that initiate cellular repair and restore balance to the body.
Her unyielding devotion to her patients has helped countless patients on the brink of giving up hope to finally improve, recover, or completely heal from a variety of severe and chronic health issues.
The post 210 – Cheating your way to good health [Podcast with Dr. Dana Cohen] appeared first on PCOS Diva.
October 9, 2024
How Dr. Vinu Jyothi and PCOS Diva Empower Women to Thrive With PCOS

[ The following article was republished from HealthNews.com; The original version of this article available here ]
Polycystic ovary syndrome (PCOS) affects close to 10% of women of childbearing age and is a major cause of infertility. Dr. Vinu Jyothi, MD, MPH, knows this struggle firsthand, having dealt with irregular periods and hormonal imbalances since her teens. She decided to turn her experience with PCOS into something meaningful by empowering other women to become PCOS Divas.
PCOS is often managed by the use of birth control pills such as clomifene, alongside recommendations for diet and lifestyle changes. However, many women feel lost when it comes to making those changes, not knowing where to start. As a result, countless women continue to suffer in silence when conventional treatments fail to improve their quality of life.
Healthnews interviewed Dr. Vinu Jyothi, the current director of PCOS Diva, which “offers a variety of programs to help women heal and feel better, no matter where they are in their PCOS journey.” In the interview, she discussed her own experience with PCOS, why conventional treatments often fall short, and how she’s helping women take a more natural, holistic approach to managing their condition and thriving.
Q: To get us started, can you briefly share how your journey with PCOS began?
A: My journey with PCOS began in my teens, marked by irregular periods, hormonal imbalances, and frustrating skin issues. At the time, I felt lost and alone, unable to understand what was happening to my body. Seeking medical help, I found that the treatment was often focused on managing symptoms rather than addressing the root cause.
Feeling frustrated and determined, I began researching PCOS and discovered that many women were facing similar challenges. Inspired by my own experience along with my expertise in medicine and public health, I wanted to empower women with PCOS. I joined PCOS Diva, a leading organization in the field following in the footsteps of Amy Medling. I feel privileged to drive PCOS Diva’s efforts to offer holistic approaches, community support, and evidence-based information to women living with PCOS.
Q: Your journey with PCOS wasn’t all rosy at the beginning. What aspects of conventional PCOS treatments frustrated you and led you to seek alternative approaches?A: When I was first diagnosed with PCOS, I felt overwhelmed and lost. Conventional therapy often felt like a one-size-fits-all approach, focusing on symptom management rather than addressing the root causes. I was prescribed oral contraceptive pills just like so many other women with a new diagnosis of PCOS that only provided temporary relief.
Frustrated by the lack of individual care and a holistic approach, I began exploring alternative strategies like dietary changes, exercise, and stress management to take control of my health and discover a sustainable approach that would improve my overall well-being.
Q: Along the journey, you found out that you had aced the PCOS game and become a Diva. Can you introduce PCOS Diva and explain what inspired you to create this movement?A: Imagine a world where women with PCOS feel confident, empowered, and supported, like a Diva. That’s the vision behind PCOS Diva. Amy, a PCOS warrior herself, founded PCOS Diva after realizing the need for a supportive community for women with this condition. Personally, as a woman with PCOS since my teenage years, I too realized that there was a need for a supportive community where women could share experiences, learn from each other, and find encouragement to live a Diva lifestyle. I wanted to provide a platform for women to feel empowered, confident, and hopeful. Following her, I joined the efforts to support this vision.
My team at PCOS Diva provides scientific insights into lifestyle changes, nutrition, and holistic strategies for managing the condition. Serving PCOS Diva has been incredibly rewarding. It has allowed me to connect with inspiring women from around the globe and make a positive impact on their lives.
Now, PCOS Diva is a movement driven by women who understand the challenges of living with PCOS and are committed to helping others overcome them. We believe that PCOS doesn’t define you; it’s simply a part of your journey. By embracing a positive mindset and making informed choices, women with PCOS don’t just survive but successfully thrive.
Q: Proper and adequate nutrition seems to be at the core of what you advocate for at PCOS Diva. Could you tell us about the PCOS Diva nutrition plan? What are its key principles?A: The PCOS Diva nutrition plan is based on the principles of whole, unprocessed foods, balanced meals, and mindful eating. We focus on nutrient-dense foods that support hormonal balance, reduce inflammation, and improve insulin sensitivity. In fact, we developed meal plans suited for each season as well: PCOS Diva Spring Meal Plan, Summer Meal Plan, Fall Meal Plan, and Winter Meal Plans.
Some of the key principles of our nutrition plans include:
Reducing refined carbohydrates and sugars: These can contribute to insulin resistance, a common issue in PCOS.Increasing fiber intake: Fiber helps regulate blood sugar levels and promotes digestive health.Prioritizing healthy fats: Healthy fats, such as avocados, nuts, and seeds, can support hormonal balance and reduce inflammation.Eating regular meals and snacks: This helps stabilize blood sugar levels and prevent overeating.Hydrating adequately: Staying hydrated is essential for overall health and can help manage PCOS symptoms.Q: In your opinion, can all women with PCOS benefit from nutrition and supplements? Is this a substitute for conventional medicine or is it a complementary approach?A: I believe that nutrition and supplements can be beneficial for many women with PCOS. By addressing underlying nutritional deficiencies and supporting hormonal balance, a well-balanced diet and targeted supplements can help improve symptoms and the overall quality of life. However, for some women, they are not a one-size-fits-all solution, so a combination of medical treatments and lifestyle modifications is essential to manage their condition effectively.
For those women, supplements alone should not be considered a substitute for conventional medical treatment. Individual needs may vary depending on specific symptoms, underlying health conditions, and other factors. They can be used as a complementary approach to support their overall health and well-being.
Q: Regarding supplements, why are they essential, and can a well-balanced diet alone meet all nutritional needs?A: While a well-balanced diet can be a great starting point, it may not be enough to meet all nutritional needs in women with PCOS. Factors such as food sensitivities, digestive issues, and increased nutrient requirements can make it difficult to get enough of certain nutrients through food alone. Supplements can help fill in the gaps and support specific areas, such as hormonal balance, insulin sensitivity, and overall health.
PCOS can often lead to nutrient deficiencies, such as vitamin D, iron, and magnesium. These deficiencies can contribute to a variety of health problems, including irregular periods, fatigue, and mood disorders. Supplements can help support hormonal balance, which is crucial for women with PCOS. For example, inositol, a nutrient found in certain foods, has been shown to improve insulin sensitivity and reduce androgen levels, both of which are common issues in PCOS. PCOS is often associated with chronic inflammation; supplements like omega-3 fatty acids can help reduce inflammation and improve overall health.
Q: What are some of the biggest challenges you’ve faced in advocating for women with PCOS?A: One of the biggest challenges we’ve faced at PCOS Diva is the lack of understanding and awareness about PCOS. Firstly, many individuals with PCOS still mistakenly believe it’s solely a body weight management issue. While body weight can be a factor, it’s crucial to recognize that PCOS is a complex hormonal disorder with a variety of symptoms.
Secondly, there’s a persistent misconception that PCOS is a minor inconvenience. It’s important to emphasize that PCOS can have significant health implications. Additionally, there’s a misconception that women with PCOS cannot conceive. While there may be challenges, many women with PCOS, including myself, have gone on to have healthy pregnancies and beautiful babies. Finally, there’s a need for more research to address the diverse experiences of women with PCOS, including women of color and those with comorbidities.
Q: What are your goals for PCOS Diva in terms of advocacy and raising awareness about PCOS?A: Our primary goal for PCOS Diva is to become a leading voice in advocating for women with PCOS. We aim to raise awareness about the condition, challenge stigma, and drive research for better treatments and support. We want to create a world where women with PCOS feel empowered, understood, and supported in every aspect of their lives.
Q: What are your thoughts on the future of PCOS treatment and research?A: I am optimistic about the future of PCOS treatment and research. With advancements in technology and increased awareness, I believe we will see significant progress in understanding the underlying causes of PCOS and developing more effective treatment protocols.
As we learn more about the genetic and hormonal factors that contribute to PCOS, we can develop more tailored treatment approaches for individual patients. Researchers are continually working to develop more effective and targeted medications that address the underlying causes of PCOS. Evidence-based research is highlighting the importance of lifestyle factors, such as diet and exercise, in managing PCOS symptoms. Emerging technologies, like gene editing and stem cell therapy, may offer promising new avenues for treating PCOS.
Overall, I’m excited about the potential for improved treatment options and a better quality of life for women with PCOS.
Q: Reflecting back on your journey, what is the one thing you wish you knew when you first had your diagnosis that would have potentially made the journey much easier?A: If I could go back in time, I would tell myself to be patient and kind to myself. The journey to healing PCOS can be challenging, but it’s important to remember that progress takes time. Don’t get discouraged by setbacks, and celebrate small victories along the way.
Additionally, I would emphasize the importance of seeking support from others with PCOS. Connecting with women who understand what you’re going through can provide invaluable support and encouragement. Finally, I would remind myself to focus on self-care. Prioritizing activities that promote your physical and mental well-being, such as exercise, relaxation techniques, and healthy eating, can make a significant difference in your journey.
My parting message to your readers is: remember, you’re not alone in this journey. There are countless women who understand what you’re going through. Seek support, educate yourself, and prioritize self-care. With the right tools and support, you can thrive with PCOS.
DisclaimerPlease note that this section includes paid content and/or native ads (hereinafter — ‘Sponsored Content’). As a responsible media publisher, we strive to maintain transparency and provide clarity to our readers regarding the nature of content on our website. Therefore, Sponsored Content is always labeled as such.Sponsored Content aims to inform and engage readers, but it typically also promotes some products, services, or brands.We encourage readers to exercise personal judgment and critical thinking when consuming Sponsored Content and/or making decisions based on it. Additionally, for health-related matters, we recommend consulting a healthcare professional. We neither endorse nor take responsibility for the use of or reliance on any information, goods, or services provided by advertisers. Learn more.We take our editorial integrity seriously. Our editorial decisions are always independent of advertisers.To report any issues related to Sponsored Content, share tips, or explore advertising opportunities on our website, please contact us here.The post How Dr. Vinu Jyothi and PCOS Diva Empower Women to Thrive With PCOS appeared first on PCOS Diva.
September 23, 2024
Disparities in PCOS – Research Survey
Green Level High School, 7600 Roberts Rd, Cary, NC 27519 USA
ABSTRACT
Polycystic ovary syndrome (PCOS) is a hormonal disorder affecting women of reproductive age. While diagnosis requires specific criteria, many women experience symptoms suggestive of PCOS without a formal diagnosis. This study aimed to characterize the experiences of women with PCOS symptoms through a survey analysis across different racial and ethnic groups.
Study Objective: To investigate the prevalence of androgenic and metabolic phenotypes among women with polycystic ovary syndrome (PCOS) across different racial and ethnic groups.
Methods: A cross-sectional study was conducted on women aged 15-55 years diagnosed with PCOS according to the modified Rotterdam criteria. Participants self-reported their race and ethnicity, and underwent assessments of androgenic and metabolic parameters.
Results: The survey revealed significant disparities in the awareness, diagnosis, and management of hormonal imbalances, particularly PCOS, across racial and ethnic groups. Asian women had lower rates of diagnosis, while Hispanic/Latinx women reported higher rates of sleep disturbances and mood disorders. Additionally, there were differences in the prevalence of skin and hair concerns among different groups.
Conclusion: Our findings highlight significant disparities in the awareness, diagnosis, and management of hormonal imbalances, particularly PCOS, across racial and ethnic groups. These disparities underscore the need for improved access to healthcare, culturally sensitive education, and targeted interventions to address the unique needs of women from diverse backgrounds. By addressing these disparities, we can promote better health outcomes for women with hormonal imbalances.
INTRODUCTION
Polycystic ovary syndrome (PCOS) is a common endocrine disorder affecting approximately 1 in 10 women of childbearing age. While the exact cause of PCOS remains unclear, it is believed to involve a complex interplay of genetic, hormonal, and environmental factors. Characterized by menstrual irregularities, hyperandrogenism, and polycystic ovaries, PCOS has a significant impact on women’s physical and mental health. Many women experience symptoms suggestive of PCOS, such as irregular periods, excess hair growth, acne, and weight gain, without receiving a formal diagnosis. Despite its global prevalence, PCOS is often underdiagnosed or misdiagnosed and many women remain unaware of the condition or do not seek appropriate medical attention. Many women are unaware of the connection between hormonal imbalances and common symptoms like weight fluctuations, mood swings, and irregular periods, leading to delayed diagnosis and potentially inappropriate treatment. This delay in diagnosis can lead to significant health consequences, including infertility, type 2 diabetes, and cardiovascular disease. Moreover, the National Institutes of Health (NIH) emphasizes the role of insulin resistance, a key component of PCOS, in contributing to obesity and cardiovascular diseases.
Previous studies have investigated the prevalence and impact of PCOS in various populations. However, there is a lack of comprehensive research exploring the experiences of women with PCOS symptoms, particularly in diverse racial and ethnic groups. Understanding these experiences is crucial for improving healthcare delivery and addressing the unique needs of women with PCOS. Moreover, studies underscore PCOS manifests differently across various ethnic groups and how cultural beliefs and practices can influence the recognition and management of hormonal imbalances. Factors such as genetic predispositions, insulin resistance, and environmental influences contribute to the development and presentation of PCOS symptoms. Studies indicate that minority women, especially Black and Hispanic women, face greater barriers to healthcare access, increasing their risk of underdiagnosis for conditions like PCOS and thyroid disorders. Additionally, the disparities in symptom presentation and diagnosis rates emphasize the importance of targeted educational initiatives to improve awareness and promote early detection. This highlights the need for personalized approaches in diagnosing and treating hormonal imbalances.
This study aims to characterize the experiences of women with PCOS symptoms through a survey analysis. By examining factors such as menstrual regularity, birth control use, weight changes, mental health, skin and hair concerns, and reproductive and metabolic health, we seek to identify common challenges faced by this population. Additionally, we aim to explore potential racial and ethnic disparities in the prevalence and impact of PCOS symptoms. The findings of this study will contribute to a better understanding of the lived experiences of women with PCOS symptoms and inform the development of culturally sensitive healthcare interventions. By addressing the unique needs of this population, we can improve their overall quality of life and reduce the burden of PCOS.
HYPOTHESIS
It is hypothesized that a significant number of women, particularly those from marginalized groups, will be unaware of their hormonal imbalances despite experiencing common symptoms like irregular periods, mood swings, and weight changes. Many women may attribute these symptoms to lifestyle factors rather than recognizing them as signs of an underlying hormonal condition. Consequently, the survey is expected to reveal gaps in both awareness and diagnosis, particularly among ethnic groups with disparities in healthcare access and education. These disparities will likely contribute to varying levels of understanding regarding hormonal health and its management.
METHODOLOGY
Study Design
We employed an online survey to evaluate women’s experience and knowledge of hormonal imbalances. All participants provided informed online consent prior to survey participation. The survey was disseminated through various social media platforms and online women’s health forums, such as Facebook groups, Instagram, and specialized health communities.
Participants
Women aged 15-55 who met the modified Rotterdam criteria for PCOS, based on self-reported symptoms in the online survey, were included. Participants came from White, Black American, Hispanic/Latinx, and Asian backgrounds. The survey questions were designed to comprehensively assess a broad spectrum of symptoms and experiences associated with hormonal imbalances. We collected data on demographics, menstrual cycles, birth control use, weight changes, mood and sleep issues, skin and hair concerns, and reproductive and metabolic health. Participants answered “yes” or “no” to each symptom and provided more details when asked. We used descriptive statistics to analyze the data.
Racial and Ethnic Groups
Participants identified themselves as Black American, White, Asian, or Hispanic/Latinx. For clarity, we excluded those who identified as mixed race such as Asian British, East Indian, Mixed Pacific Islander/White, Portuguese Canadian, Fijian of Indian descent (Pacific Islander), or Native American/Alaska Native due to small sample sizes.
Data Analysis
We examined the survey responses to find patterns and differences among various demographic groups. To ensure the survey’s quality, we took steps like testing questions beforehand and including diverse participants to capture a wide range of experiences. This approach aims to improve our understanding of how different racial and ethnic groups perceive and manage hormonal imbalances.
RESULTS
The survey results demonstrate significant disparities in the awareness and diagnosis of hormonal imbalances, particularly PCOS, across racial and ethnic groups. The racial/ethnic breakdown was 75% White, 5% Black American, 5% Hispanic/Latinx, and 23% Asian.
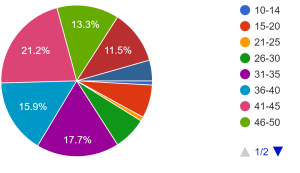
Race Age groups
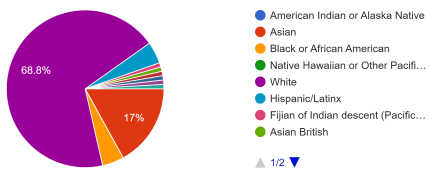
Among White women and Hispanic/Latinx, 90.7% and 80% respectively reported having PCOS, compared to only 17.4% of Asian women and 40% of Black American women (Figure 1A). Additionally, diabetes or insulin resistance rates varied significantly, with higher rates among White and Black American women. Diabetes or insulin resistance was less prevalent, with the highest rate among Black American participants (60% Black American) and White participants (49.3%). A least prevalence (4.3%) was reported among Asian participants (Figure 1B). This suggests possible underdiagnosis or lack of awareness in these minority groups.
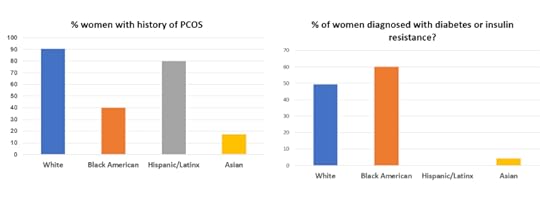 Figure 1A (left) and 1B(right)
Figure 1A (left) and 1B(right)
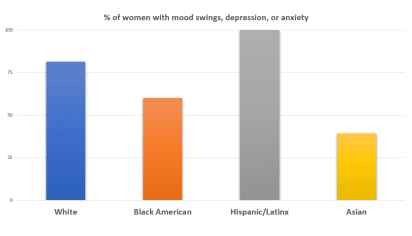 Figure 2
Figure 2We saw similar trends for mood swings, depression and anxiety with White women reporting higher rates (81.3%) than Black (60%) or Asian women (39.1%) participants (Figure 2).
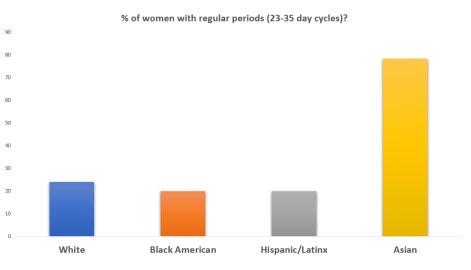 Figure 3
Figure 3The survey results show that Asian women have the highest percentage (78.3%) of experiencing frequent regular periods, followed by White (24%), Black American (20%), and Hispanic/Latinx (20%) women (Figure 3).
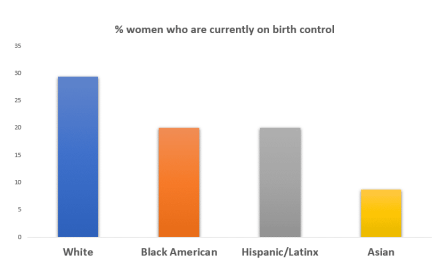 Figure 4.
Figure 4.Among all participants, 24% of women reported using birth control. The majority of women from White (29% White]) background reported currently using a birth control compared to a low percentage of Asian women (8.7%). Only a moderate percentage (%20) of Black American and Hispanic/Latinx participants reported using a birth control (Figure 4).
Majority of Hispanic/Latinx women (100%) and White women (81%) reported mood swings, depression, or anxiety, as compared to only 60% of Black American women. However, fewer Hispanic/Latinx women were diagnosed with thyroid disorders compared to White or Black American women, indicating a possible diagnosis gap despite symptoms (Figure 5A and 5B).
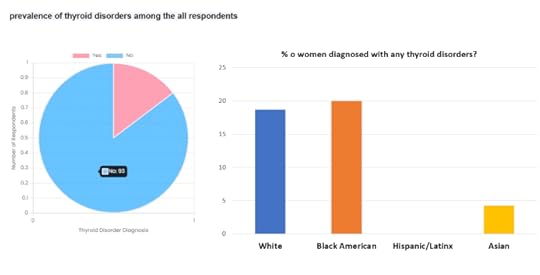 Figure 5A (left) and 5B (right).
Figure 5A (left) and 5B (right).
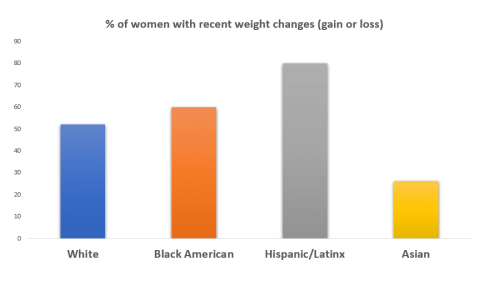 Figure 6.
Figure 6.
A significant proportion of women across all racial/ethnic groups reported experiencing recent weight changes (gain or loss), with the highest prevalence among Hispanic/Latinx participants (80% Hispanic/Latinx) (Figure 6).
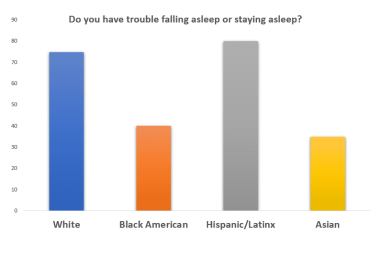 Figure 7.
Figure 7.Sleep disturbances, such as difficulty falling or staying asleep, were also common across all groups, but again, Hispanic/Latinx women had the highest prevalence (80%). Asian and Black American women reported the lowest rates of sleep disturbances, at 35% and 40%, respectively (Figure 7).
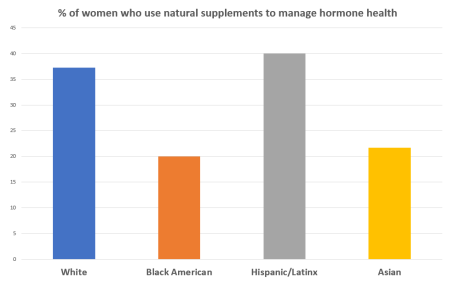 The data also reveals differences in the use of natural supplements, with White (37.3%) and Hispanic/Latinx (40%) women more likely to use them compared to Asian women (21.7%). This might suggest varying awareness of natural treatments or cultural preferences in health management (Figure 8).
The data also reveals differences in the use of natural supplements, with White (37.3%) and Hispanic/Latinx (40%) women more likely to use them compared to Asian women (21.7%). This might suggest varying awareness of natural treatments or cultural preferences in health management (Figure 8).
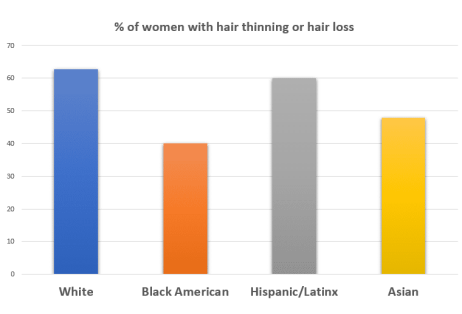 Figure 9.
Figure 9.Most women reported skin problems, such as acne or dryness, and hair issues, such as thinning or loss. However, there were significant differences between racial and ethnic groups. White women reported these issues most frequently (77%), followed by Hispanic/Latinx women (60%), while Black American women reported them less often (40%). Hair loss or thinning was more common among White and Hispanic/Latinx women (63% and 60%, respectively) compared to Black American and Asian women (40% and 47%) (Figure 9).
Among all surveyed women with PCOS, we observed an interesting age-related pattern in fatigue, hot flashes,, headaches, stress related responses as seen below Figure 10.
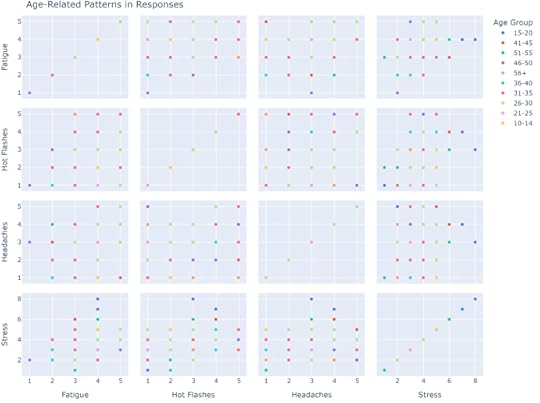 Figure 10.
Figure 10.
These findings support the hypothesis that a significant number of women, especially from minority groups, remain unaware of their hormonal imbalances. The disparities in symptom reporting and diagnosis across racial groups highlight the influence of cultural, socioeconomic, and healthcare access factors on the awareness and management of these conditions.
DISCUSSION
The results of our survey underscore significant disparities in the awareness, diagnosis, and management of hormonal imbalances, particularly polycystic ovary syndrome (PCOS), across racial and ethnic groups. These disparities highlight the need for improved access to healthcare, culturally sensitive education, and targeted interventions to address the unique needs of women from diverse backgrounds.
Many women live with untreated or undiagnosed symptoms, significantly impacting their quality of life. Symptoms like weight gain, mood swings, hair loss, and irregular periods are often dismissed as stress-related or lifestyle factors, especially in cultures where reproductive and hormonal health are stigmatized. This lack of awareness, coupled with systemic barriers to healthcare, can lead to delayed diagnosis and treatment, increasing the risk of long-term complications.
Our findings demonstrate a substantial gap in awareness and diagnosis of PCOS, particularly among minority groups. Asian women had significantly lower rates of PCOS diagnosis compared to White and Hispanic/Latinx women, suggesting underdiagnosis or lack of awareness. We could hypothesize that Asian women may have a lower genetic predisposition or different metabolic factors that contribute to PCOS. However, this is just one possible interpretation, and other factors could also be at play. The sample size for Asian women might be smaller, potentially limiting the generalizability of the findings. These disparities may be influenced by cultural factors, language barriers, and limited access to healthcare.
The survey revealed differences in the reporting of symptoms associated with hormonal imbalances, such as mood swings, depression, anxiety, and sleep disturbances. Hispanic/Latinx women reported higher rates of sleep disturbances and mood disorders, while Asian women reported lower rates of these symptoms. These variations may be attributed to cultural factors, differences in symptom presentation, or varying levels of stress and social support.
The data on birth control use and natural supplement usage highlights disparities in healthcare access and preferences. Asian women had lower rates of birth control use, potentially indicating barriers to accessing reproductive healthcare. The higher rates of natural supplement use among White and Hispanic/Latinx women may reflect cultural preferences or a desire for alternative approaches to health management.
The survey also revealed differences in the prevalence of skin and hair concerns across racial and ethnic groups. White women reported higher rates of skin and hair issues, while Black American women reported lower rates. These disparities may be influenced by genetic factors, cultural beauty standards, and access to skincare and hair care products.
In countries with limited healthcare access, women are even less likely to receive appropriate medical care or hormonal screenings. Healthcare infrastructure, socioeconomic status, and cultural beliefs further contribute to the underdiagnosis of hormonal disorders. In many communities, these issues are not considered medical priorities, leading to women delaying seeking medical help until symptoms become severe. The survey results mirror this global underrecognition, as women from minority groups were less likely to be diagnosed with PCOS or related disorders despite reporting similar symptoms.
To address this global issue, education and awareness campaigns are crucial. These campaigns should focus on helping women recognize the symptoms of hormonal imbalances and encourage early treatment. Additionally, healthcare providers need to improve their diagnostic approaches by regularly screening for hormonal disorders, especially among women with symptoms like irregular periods, weight fluctuations, and mood disturbances. In countries with limited healthcare access, mobile health units and telemedicine should be optimized to reach women who may otherwise remain undiagnosed.
Treatment options should also be made more widely known. While lifestyle changes can help manage some symptoms, many women may benefit from hormonal therapies, supplements, or medication. Alternative and natural supplements are also becoming popular for managing hormonal health, as evidenced by the survey. Women should be encouraged to work closely with healthcare professionals to develop personalized treatment plans.
LIMITATIONS
This study is limited by its self-reported nature and lack of clinical diagnosis and comprehensive statistical analyses for PCOS. Additionally, the sample size may not be generalizable to the entire population with PCOS symptoms.
CONCLUSION
This survey provides valuable insights into the prevalence of menstrual irregularities, weight changes, mental health concerns, sleep disturbances, and skin and hair problems among this population. Racial/ethnic disparities were observed in some areas, suggesting potential healthcare access or cultural influences.
While the data suggests a potential difference in PCOS prevalence between Asian and White women, more research is needed to fully understand the underlying reasons. Factors such as genetics, lifestyle, and cultural influences may play a role. It’s essential to consider these factors when interpreting the findings and developing targeted interventions for PCOS prevention and management. Further research is needed to explore the underlying mechanisms of these symptoms and develop culturally sensitive management strategies.
In conclusion, our study provides valuable insights into the disparities in hormonal imbalance awareness, diagnosis, and management across racial and ethnic groups. By addressing these disparities through improved access to healthcare, culturally sensitive education, and targeted interventions, we can promote better health outcomes for women from all backgrounds.
IMPLICATIONS AND FUTURE DIRECTIONS
Overall, addressing the global burden of hormonal imbalances requires a multi-faceted approach, including increasing access to affordable healthcare, reducing stigma around women’s health issues, and creating a more open educational environment regarding hormonal imbalances. By addressing these issues early, we can prevent more severe health problems and empower women to lead healthier and more fulfilling lives.
Our findings emphasize the need for culturally sensitive education and awareness campaigns to address the disparities in hormonal imbalance awareness and diagnosis. Healthcare providers should be trained to recognize the diverse presentation of symptoms and to provide culturally appropriate care for women from different backgrounds. Future research should explore the underlying factors contributing to these disparities, including socioeconomic status, access to healthcare, cultural beliefs, and genetic differences. Targeted interventions, such as culturally tailored educational programs and community-based support groups, may be effective in improving the health outcomes of women with hormonal imbalances, particularly those from minority groups.
The post Disparities in PCOS – Research Survey appeared first on PCOS Diva.







