Ashwin Naik's Blog
October 9, 2020
Why Communities Should Lead the Mental Health Movement in India
A 500-year old dargah (Islamic shrine) in Unava, Gujarat, is today the site of a quirky merger of faith healing and modern psychiatry. For centuries, local legend has credited the Hazrat Saiyed Ali Mira Datar dargah with the power to cure various mental illnesses. But since 2008, the dargah’s mujavars (traditional healers) have been trained by experts to watch for signs of mental illness in patients. Any patient exhibiting warning signs is escorted to a clinic within the shrine’s premises, where he or she is examined and treated by doctors. For their part, the doctors ensure that the treatment does not interfere with the rituals prescribed by the mujavars. And everyone is satisfied.
From a Western perspective, Gujarat’s ‘Dava-and-Dua programme’ could seem odd, even unscientific. However, the programme’s success underlines the benefits of innovative community-based mental health models for developing countries like India. According to the National Mental Health Survey (NHMS), one in seven Indians will experience mental morbidity during their lifetime. Yet, the treatment gap for mental disorders is as high as 85%. India’s huge population and far-flung villages, its under-funding of health, low public awareness, and policy implementation gaps pose great challenges in taking mental health services to the last mile.
However, community psycho-social interventions can effectively complement hospital-based care for people living with mental conditions in less-affluent countries. The World Health Organisation states quite clearly that “there are no persuasive arguments or data to support a hospital-only approach”, adding that “low-resource countries should focus on establishing and improving mental health services within primary care settings, using specialist services as a backup.”
Benefits of community-led mental health
One of the biggest challenges to accessing mental health services in India is distance. While India has had a District Mental Health Programme since 1996, the NMHS calculates that affected families have to spend Rs 1000-1500 per month to access mental health services. These high costs can deter patients, especially from lower-income backgrounds, from seeking treatment.
The obvious solution? Transfer some of these services to members of the community—ASHA workers, local healthcare professionals, NGOs, and so on. Given that India has less than 1 psychiatrist per lakh population, it is unfair to expect doctors to shoulder the entire burden of patient care. The solution lies in training local health workers or volunteers who can go door-to-door in their neighbourhoods, and provide at least a basic level of mental health support and counselling.
There are many successful examples of community-led mental health initiatives in India. These include the work of Sangath in Goa, the Atmiyata campaign in Maharashtra and Gujarat, and the Mental Health Action Trust (MHAT) in Kerala. Catering to some of the most deprived sections of society, these initiatives use trained volunteers to serve as an interface between doctors/hospitals on one hand, and patients on the other. For instance, in Maharashtra, Atmiyata’s volunteers have covered 14,000 residents of rural Nashik and connected nearly 70% of the affected people to public health services. Another 10 lakh people have been covered in Gujarat.
Community-based healthcare can also be extremely cost-effective by putting responsibility for patient care into the hands of the latter’s community. For instance, MHAT’s volunteers include homemakers, shopkeepers and farmers. These volunteers regularly visit and keep tabs on patients with severe mental disorders living in their neighbourhoods. The patient details are then shared with MHAT’s team of experienced psychiatrists, who use video-conferencing or telephone to speak to the patients, and prescribe the required medicines. The funds for the initiative are raised by the volunteers themselves, making it free for the 4000-odd beneficiaries across Kerala.
Besides making mental health easier to access and cheaper to provide, community-based services also see a greater level of acceptance. This is because the volunteers use local language and idioms, keep context and culture in mind (as in the Unava example). A great global example of this is the ‘Friendship Bench’, first launched in Zimbabwe. A local psychiatrist, trying to think of solutions for the massive shortage of mental health professionals, chanced upon the idea of setting up benches where specially-trained ‘grandmothers’—elderly Zimbabwean women—would offer a listening ear and helpful advice to people with mental health issues. The doctor’s idea overcame a lot of initial scepticism, and eventually became a huge initiative that was replicated in other African countries, and even in the US!
So why did it work? It turned out that the comforting presence of the elderly women, and the relatively casual setting—a bench under a tree in the open—allowed patients, ‘referred’ by friends, family or health workers, to open up about their problems. What’s even better is that the grandmothers themselves felt a powerful sense of purpose due to the impact of their work, and this improved their own mental health!
On the eve of the World Mental Health Day 2020, there is a global push to invest in better mental health. Governments and policy makers must, however look outside of formal medical sector for solutions. Community mental healthcare might be a relatively unexplored area. However, it also has tremendous potential for providing a healing touch at the grassroots level, especially in these troubled times. For centuries, a person’s well-being was a ‘shared contract’ between the individual and their tribe, village or community. Going back to that tradition seems the obvious solution for the problems humanity faces today. Surely, we can all benefit from a bit of “Dava and Dua” in these times.
— Published on October 8, 2020 on Thrive Global
June 8, 2020
Bloomberg Quint – Mental Health and COVID19
More Attention, No Institutional Mechanism
For every million people in India, there are just three psychiatrists, and even fewer psychologists, according to a 2015 WHO report. Mental health professionals discontinuing appointments during the lockdown compounded the problem for patients. Add to that the stress and anxiety from job losses, loan defaults, and the general uncertainty.
Covid 19 has exacerbated the environment for mental health patients who were underserved to begin with, Ashwin Naik, founder of Manah Wellness, said. But the lockdown has brought these issues front and centre and people are paying more attention to them, he said. Naik’s company has tied up with several NGOs to provide a mental health helpline—called ‘Let’s Talk’.
Various agencies have seen that there is a 20-30% increase in the number of calls and cases that have come to them. One of the big challenges we foresee is that this will not end with the lockdown—the impact of this will stick for months and years. Ashwin Naik, Founder, Manah Wellness
The maximum number of calls, he said, has come from two categories: small business owners and adolescents/young people, particularly those who are entering the job market for the first time.
Read more at: https://www.bloombergquint.com/business/how-indias-healthcare-startups-have-innovated-during-covid-19
Copyright © BloombergQuint
June 3, 2020
How startups should ensure mental wellbeing of employees post lockdown
Nine out of ten employees are apprehensive and anxious about their return to workplace and are worried about their health and safety. This was recently revealed by a survey conducted by health-tech community product FYI and MindMap Advance Research.
As we enter the last phase of lockdown and enter the unlock phase 1, the most common question on every startup leader’s mind is what do we do once we return to work? How can we take care of our team’s needs, assuage their apprehensions, and build a sense of psychological safety.
Startup leaders have it especially tough given the uncertain economic conditions and the massive pressure to conserve cash. News about layoffs and restructuring in startups has also created a lot of apprehension about jobs, future, and stability in many startups.
While it is not easy to have all the answers, the most important thing at this point is to start with empathy.
Making sure that our teams feel they are being heard and understood, giving them space to get readjusted to the workplace, and recognising the emotional stress the last few weeks have brought to everyone will help set the stage for this long journey ahead.
The following guidelines can help leaders be prepared for the conversations coming up in the next few weeks.
Clear and honest communication with the team
While clear communication is always appreciated, never has been a better time than now to have clear and honest discussion with your teams. Given what people have been reading in the news and watching online, most people know these are unusual times, and they understand that the next two years will be tough for everyone.
Having honest and clear conversations will set the tone for finding solutions, both short and long-term ones. It is important for the team to understand where they really stand and then jointly plan the way forward. Putting yourself in their position shows both in your words and in your actions will go a long way.
Assure emotional well-being and support
The biggest casualty of the viral pandemic has been mental health. As the lockdown is ending, the mental health epidemic is just emerging. Over the next few months, we will see a tremendous increase in emotional stress as a long term impact of the lockdown. What teams need now is a reassurance that their emotional wellbeing is paramount, and as an organisation you are committed to it.
Leadership teams, along with your human resources colleagues, have the responsibility that they ensure every person in the organisation knows that if they need emotional support, the organisation will stand with them. There are professional wellbeing organisations that can provide this support, as well as free resources during COVID-19 that offer confidential and free support, like Let’s TALK and NIMHANS.
Re-assess workplace settings
Social distancing is now on everyone’s mind. How do we ensure that we maintain physical distancing while not losing the social connections? Having worked from home for many months, everyone is looking forward to being face to face and reclaiming their social connections. Making sure that the workplace is now conducive to the new environment is critical.
The natural tendency would be to build more barriers to prevent infection from spreading. While that is indeed required, let it not be at the cost of social wellbeing of your colleagues.
Doing a mental wellbeing assessment in the first week of post lockdown will give insights to leaders on what are the top three to five key issues that is on everyone’s mind. Programmes can then be delivered to allay those fears, address those concerns or build resilience to combat those issues.
Look out for early warning signs
Not everyone handles emotions the same way. Building organisational capacity to detect early warning signs and helping colleagues in coping with the evolving environment will be very extremely critical. Special attention to be paid to vulnerable people who might have an ailing family member at home or have a family member who is at the frontlines of the pandemic, treating or taking care of patients.
Having access to a psychology professional who is available on phone or WhatsApp, when it is needed, for every member of the team, which is explicitly communicated to the team, is one way to build this early warning and support system. Providing coaching and counseling support to team members as an ongoing support mechanism would also help them build the resilience for years to come.
While the pandemic is certainly not over, there is an increasing realisation around the world that we have to learn to live with this virus, and many more like this one. Business leaders around the world are accepting this new reality and developing the mindset to adapt to this new normal.
As we settle into this new normal, mental wellbeing of each one of our team members is going to be on the top of every leader’s agenda.
Equally important will be for leaders to focus on their own wellbeing and take time out to focus on self-care. Self-care might involve building a mindfulness or exercise routine, or working with a coach who can help with building a long-term plan for mindset change.
One of the top causes of anxiety among startup founders is the desire to put up a brave face when things are not looking good. So it is imperative that leaders prioritise self-care for themselves along with their teams as they navigate this new normal. (Edited by Megha Reddy)
Read more at: https://yourstory.com/2020/06/startups-ensure-mental-wellbeing-employees-post-lockdown?utm_pageloadtype=scroll
May 18, 2020
As India’s lockdown ends, a mental health crisis is just beginning
Only through local, community-based responses will India find the capacity to cope with this unfolding crisis.
Here are three evidence-based approaches that can unlock the power of communities in this fight.
India witnessed the largest containment experiment in history, when – on 25 March – its 1.3 billion citizens battened down their hatches in an attempt to flatten the COVID-19 curve. The lockdown may now be ending but – as is happening across the globe – a new epidemic is now emerging. According to a survey conducted by the Indian Psychiatry Society, within a week of the start of the lockdown, the number of reported cases of mental illness in India had risen by 20%.
In the weeks and months ahead, India will suffer from a massive mental health crisis due to unemployment, alcohol abuse, economic hardship, domestic violence and indebtedness. While this will affect most of the population it will disproportionately affect the poor, most vulnerable and marginalized groups.
Have you read?
How India’s rural poor are coping with the coronavirus lockdown
Why India has the upper hand against COVID-19
India, Pakistan ease restrictions for some small businesses amid lockdown
“At-risk populations include the 150 million with pre-existing mental health issues, Covid-19 survivors, frontline medical workers, young people, differently abled people, women, workers in the unorganized sector, and the elderly,” says Nelson Vinod Moses, a leading suicide prevention advocate in India.
When we launched a volunteer mental health support helpline – Let’s Talk – in early April, we knew we needed as many resources as possible to support existing efforts led by state governments and other civil society organizations. Based on our experience fielding calls from people in distress, we believe India’s already overburdened mental health machinery will be unable to handle this unfolding situation, and will need to leverage the power of communities with locally devised, evidence-based solutions. Here are three:
1. Destigmatization: COVID-19 has created a great deal of stigma mainly through a lack of awareness about how the disease spreads and how it attacks the human body. In many cities, healthcare workers, who are treating COVID-19 patients during the day, have been forcefully evicted from their homes out of fear that they may be bringing the virus back at night. People who tested positive are being shunned in apartment complexes by their resident associations.
The entire social distancing narrative has to be rebuilt. It’s encouraging to see how some early COVID-19 survivors turned to social media to share their experiences in order to build confidence amongst others. Maybe there is an opportunity to train the more than 19,000 Indians who have now recovered, and to turn them into COVID-19 champions – equipping them to serve as buddies for people who are now feared to be positive or are under suspicion. These champions, having experienced the stress first-hand and having recovered, are the right people to lead this change.
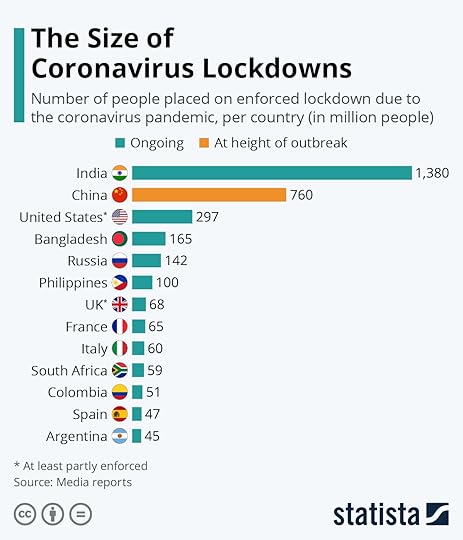
The scale of India’s lockdown is staggering
Image: Statista
2. Community infrastructure for support: Even with a team of more than 300 volunteers at Let’s Talk, we are acutely aware that it is impossible for us to provide long-term support to the community. Neither can India’s formal mental health system, which has a limited number of specialists; 9,000 psychiatrists for 1.3 billion people. Shekar Saxena, former firector of the WHO’s Mental Health Division, has said: “Mental health systems have always been very scanty in India and during this time, the gap between what is needed and what is available has widened markedly.”
The real need is to build community-based capacity in order to handle local issues long after the acute phase of the epidemic. A small team of peer counslelors working under a local administrator and trained on established models – such as Dr. Vikram Patel’s Sangath or the Atmiyata model by Centre for Mental Health Law and Policy (CMHLP) – might be the way forward. This will require a close partnership between civil society, local administration, and a standardized training and technology backbone, if it is to deliver consistent quality support. Local anchors will build accountability and ownership, and contextualize it for their own surroundings. Unless the community is empowered to take care of itself, we are staring at an ever-growing shadow of mental distress which will last much longer than the pandemic.
3. Building resilience amongst adolescents and young children. With schools closed for the past eight weeks, 253 million adolescents in India are in limbo, stuck with families unsure about their financial future, a lack of personal space, and most importantly separated from their friends. They are exposed to widespread fear fuelled by the rapid spread of the virus, compounded by constant news chatter about death and disease which creates uncertainty and apprehension about their loved ones. Many of the community support systems outside of the families have become unavailable, particularly for young girls, and domestic violence is on the rise. For an entire generation to grow up in these conditions, with no clear answers for the foreseeable future, is unprecedented and will have a significant impact on their worldview.
For adolescents, it is reset time. It is time to build mental wellbeing and resilience into schools, the community, and their families. We need a systemic approach to build the demand for mental wellbeing, just as we broadly introduced sports into schools in the late 1990s. The Indian government’s Rashtriya Kishor Swasthya Karyakram (National Adolescent Health) programme has been reconfigured to go beyond its initial remit of sexual and reproductive health. Since February this year, the programme’s focus has been updated to include outreach by counsellors, facility-based counselling, social and behavioural change.
While we try to manage the urgent task at hand – containing the virus – the long-term wellbeing of adolescents might fall by the wayside. But to let it do so would be a devastating mistake. As UNICEF has put it: “The stakes could not be higher. If not adequately or appropriately addressed, the mental health consequences for a generation of children and young people could far surpass the immediate health and economic impact of the COVID-19 pandemic, leaving long-term social and economic consequences in its wake.”
Share
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
Written by
Ashwin Naik, Healthcare Entrepreneur and Author, The Healthcare Gamechangers
The views expressed in this article are those of the author alone and not the World Economic Forum.
December 3, 2019
BILL GATES MEETS NEW-AGE HEALTHCARE LEADERS FROM INDIA: 3 TAKEAWAYS
Read More – https://www.voiceofhealthcare.org/201...
August 15, 2019
Dignity for Self and for Each Other
”Dignity is our inherent value and worth as human beings; everyone is born with it.”
In this world increasingly divided by mistrust and hate, dignity for each other and ourselves is getting sacrificed. The most fundamental and human thing about all of us is our dignity. As a matter of fact, United Nations acknowledges this in the preamble for Human Rights.
Add alt text
At the 2006 World Economic Forum, three Young Global Leaders (YGLs) sought to better understand the root cause of the violence, intolerance and injustice in our world. Their conclusion: a fundamental lack of dignity and recognition of our shared humanity. They came to the realization that the lack of a real understanding of the concept of dignity and the recognition of our shared humanity is at the heart of so much conflict and polarization.
Determined to unite more people in the belief that everyone deserves to live a life of dignity, these young leaders — Crown Prince Haakon of Norway; John Bryant, CEO and Founder of Operation HOPE; and Pekka Himanen, author, professor and advisor to the former Finnish President Martti Ahtisaari — launched Global Dignity with a workshop in one small classroom in Switzerland. Bishop Desmond Tutu and RIchard Branson joined the school visit, and were so moved by the experience, that both signed on as members of the new “Honorary Board” and Global Dignity was founded.
Global Dignity has since grown to a 70-nation-strong network of volunteer educators, civil society and business leaders, working to strengthen dignity-based values among young people in their communities. Through its annual Global Dignity Day in October and in year-round Dignity Workshops, Global Dignity reached a record 680,000 young people in 2017.
On auspicious occasion of India’s Independence Day, I am excited to start my association with Global dignity as Country Chair for India.
Global Dignity engages young people in understanding the values and principles behind what “dignity” means and aims to inspire the next generation to address the major challenges of our time by making positive change in their own communities.
The organization’s work is guided by a simple set of principles—that every person:
1. Has the right to pursue their purpose and meaning in life, and to reach their full potential.
2. Deserves to live in societies that provide humane access to education, health, income and security.
3. Should have their life, identity and beliefs respected by others.
4. Has the responsibility to create the conditions for others to fulfill their potential, acting to strengthen the dignity of others, building a foundation of freedom, justice and peace for this – and future generations.
5. Can put dignity into action by standing up against injustice, intolerance and inequality.
Add alt text

Apart from promoting dignity throughout India on a national level, Global Dignity India will also be recognizing young people around the country as Global Dignity Fellows who will become ambassadors of Global Dignity India and embody the core values of Global Dignity by living, practicing and teaching dignity to visiting schools and others organisations in their community.
To get involved and support Global Dignity India, or to know more, visit
www.globaldignity.org/india or email globaldignity@innovadis.in
July 14, 2019
Brave New Healthcare, where “Everyone Plays”?
One of the biggest challenges in the healthcare system is that it vests disproportionate power in the hands of a few – the medical practitioners. Doctors are at the top of the knowledge hierarchy in the system and hence, wield significant power in decision-making, relegating the rest of the players to marginal roles of following orders.
A patient, during her journey through the healthcare systems across the world however, interacts with the doctors just around 10% – 25% of his time. Most of the time, the interaction is with nurses, technicians, support staff and administration. Given so much of the patient experience and wellbeing is linked to what happens in the non-doctor interaction period, it is time to question the power equation in the system.
Healthcare systems around the world are unlikely to change unless we address these issues head on. And I don’t mean just more delegation to the non-doctor teams; it is truly the shift of power which is needed, the power to make decisions, the power to override decisions and ultimately, the power to set priorities for their organizations. I would wager that a truly transformative healthcare system would be run entirely by nurses, with doctors and other providers reporting to them. Of course, we need more nurse practitioners who practice primary care, more nurse administrators who run hospitals, and so on. But the key here is to build a system where decision-making or power shifts from doctors to other players in the system: a system where everyone plays.
Unless the power shift happens in a manner that it addresses these pressing concerns of power shift, awareness and preventive care, we are unlikely to see changes in the outcomes, in spite of the billions of dollars being pumped into improving healthcare each year. Unless everyone plays and towards a common goal, change is difficult.
In my book – The Healthcare Gamechangers, you will see how Dr. Rushika Fernandopulle in the United States has built just such a system with self-organized units of nurses and customer care executives that provide primary care in their neighborhood, or how Edith Elliot is empowering patient attendants and their families to take control of their own health and be ambassadors of correct information in their communities, or how Dr. Suresh Kumar is training volunteers in the community to self-organize and care for their loved ones. Be it palliative care, preventive care or immediate care, involving everyone else apart from a doctor is the need of the hour. Each nurse, volunteer, or staff can make a difference to the life of another human being, patient or not. Every healthy person educated and made aware is one potential patient averted, perhaps one family of potential patients dodged. And though this might appear to be a small number, it is substantial when we calculate the positive ripple effect that such information can bring about.
Each of these game changers is chipping away at the old system in their own way, battling a different devil, building capacity, shifting power and ensuring everyone plays, one person at a time.
Dr. Fernandopulle and Iora Health are redefining how primary care is played out. Today, insurers tend to influence medical decision-making, which is absolutely wrong. By taking complete charge of the person’s health, not just the outcome of a consultation, Iora Health is changing the outcomes right at the primary healthcare level, avoiding expensive, invasive and often unnecessary, procedures, reducing healthcare expenses and improving overall healthcare. Not just this, there is greater job satisfaction for the entire team of caregivers that attends to a patient right at the primary care level, making the person’s goals for their health and life, their mission. In Dr. Fernandopulle’s model of healthcare, not just the primary caregiving doctor, but nurses, behavioral coaches, psychologists, nutritionists and the person himself plays.
Edith Elliott of Noora Healthcare identified an unexpected ally in the patient’s recovery process — their attendants. By training the patient’s friends and family who are waiting in the hospital as the patient gets better, Edith is not just empowering the immediate caregivers with correct knowledge to reduce complications and expedite recovery, but also sending these persons, armed with accurate medical information back to the community, where usually myths and misinformation abound. In Edith’s model, friends and family participate and play towards better health for the community at large.
Dr. Suresh Kumar and the Neighborhood Network of Palliative Care is breaking down institutionalized palliative care to mini local armies of self-motivated volunteers that are trained to care for those in need from their own local community. The safety net of doctors and nurses that drive the decision-making in this model in Kerala, India, is truly delivering health with care. Using the fuel that motivates volunteers each day, Dr. Kumar has channelized this caring concern to help reduce complications, improve outcomes, provide gentle but accurate palliative care. In Dr. Kumar’s model, local volunteers and nurses play to give better end-of-life and palliative care to their very own community.
What Shifts when Everyone Plays
Decision making: Select few to distributed
When people organize themselves into smaller teams that can decide what’s best for the people they are caring for, the care delivered is much more precise, it can address issues being missed by bureaucratic hierarchy sitting miles away, and is much faster. This can mean a world of difference as far as a person’s health is concerned.
Power: At the top to the front lines
A significant amount of power is a must for every person who has a responsibility to ensure that they are doing complete justice to the job at hand. Their opinion matters.
Organization structure: Hierarchical to flat structure
A flat world might be preposterous as far the Earth is concerned, but in healthcare, it means more rapid decision making, faster execution and individualized healthcare.
Organizing principle: Command and control to self-organizing
Having rules is great and unavoidable when dealing with masses. But if rules become suffocating enough that they choke creativity, individuality, and optimization at the cost of consistency, it’s time to do away with them.
Structures: Formal employment to informal associations
The way care is delivered matters. Clean but cold environments that have all but a precisely calculated amount of care being delivered isn’t the best for recovery. The term ‘healing touch’ was coined for a reason.
May 8, 2019
Primacy Health Care is Care First, Health Second
[image error][image error]  This post is part of a series on
The Healthcare Gamechangers
.
Read all the stories in this series here.
This post is part of a series on
The Healthcare Gamechangers
.
Read all the stories in this series here.
In the modern day of doctor-patient confidentiality and the computerization of medical records, there is little chance of a whole family visiting a practice for advice, or the merrygo-round of doctors being able to spot and act upon a root cause from people who live in the same place. The ‘sticking plaster’ solution gets people back on their feet again and allows them to get on with their life until the next illness crops up, but does nothing to provide or promote an environment that makes these illnesses less likely. In many parts of the world, especially the poorer parts, there has to be a sea change in how medicine is administered. This is where pioneers like Vera Cordeiro come in.
Saúde Criança Association (ASC), is an independent social organization founded by Dr. Vera Cordeiro in 1991 in Rio de Janeiro, Brazil that pioneered an innovative methodology to assist poor families that have a sick child undergoing treatment at a public health facility. The crisis becomes real when the pre-existing challenges of poverty worsen with the need to care for the child’s health, threatening the family’s integrity even further. ASC promotes self-sufficiency of Brazilian families with children suffering from acute and chronic disease typically linked with poverty. Saúde Criança’s program, the ‘Family Action Plan’ (FAP), adopts an innovative methodology: it is based on the principle that poverty is one of the important causes of disease. The causes of poverty and illness are multidimensional. The plan, which consists of a multidisciplinary team exerts integrated actions in the areas of health, education, citizenship, housing, and income, and is built based on each family’s needs. Besides overcoming the immediate difficulties inherent to the child’s post-hospitalization phase, the entity’s goal is to offer orientation and opportunities so that the family unit has its rights guaranteed and can enjoy a reasonable quality of life.
Saúde Criança fights for social inclusion by promoting human development. The crucial element of the methodology and one of the keys to its success is the family’s active participation elaborating the plan, objectives, and goals to be met during each phase over the two years in which it is part of the program. Every family is assisted individually, according to their needs and potential, during a period of approximately two years. The family’s progress is tracked during regular meetings with the Saúde Criança team with the objective of helping the family achieve dignity and autonomy.
Read more about Saúde Criança and Dr Vera Cordeiro in my book “The Healthcare Gamechangers” now available as kindle e-book worldwide and paperback in select markets.
October 1, 2017
Healthy Behaviour – Is our biggest problem the way we communicate?
This post is part of a series on The Healthcare Gamechangers. Read all the stories in this series here.
The story of Nalini Saligram and Arogya World
Healthcare has been developing along one line for centuries. We look to help people far too late in the process to have any meaningful intervention. Once someone presents with type 2 diabetes, for example, then the horse has already bolted. Not only are all attempts from then on about managing a disease rather than curing it, but the time and money needed to do this by far outweigh earlier intervention. It would test the skill of any doctor to not only perform an operation or prescribe the right treatment, but also motivate people to do the right things. This is actually one of the key elements in changing behaviors. I believe that there are two strands to this,
The education to understand what affects health and how to act.The motivation to put this education into action.Telling is speaking to the brain. It is pointing someone in the right direction. It is cold and hard. Selling is speaking to the heart. It gets people off their seat and interested in what you have to say.
Medicine is almost completely focused on the telling part. We tell people to stop smoking. We tell people to lose weight. We tell people to get more exercise. We tell people to cut down on alcohol, sugar, salt and many other things. But we don’t sell often enough. Once again, we see an area of healthcare that doesn’t perform in the optimal way. People may understand all the ‘tell’ arguments you give them, but without the ‘sell’ motivation to do anything, you are wasting your breath.
We have also seen how moving the care away from the daunting and centralized hospital into the community has a big impact on the consumption of healthcare. So why do we insist on excluding people from the conversation?
Communication is vital to reach people earlier in the cycle of wellness. But without the right techniques to reach people, these attempts will not be as effective as they can. Just communicating with people in their own environment is a step in the right direction, but this needs to be effective communication to make the kind of sea change that is required.
Take Nalini Saligram’s work in India.
Diabetes is a problem across the country of India, where there are more than a billion people and little access to healthcare education. Add into the mix the poverty that is rife in many parts of the country and you have a problem that is bubbling up for the near future. And it isn’t just the poorer people that are facing issues. The growing middle class in the country are working longer hours and consuming an ever-poorer diet. Conditions like type 2 diabetes and heart disease are affecting the people of India in bigger numbers each year.
An estimated 20 per cent of Indians have at least one chronic condition. 69 plus million Indians live with diabetes, 77 million are said to have pre-diabetes and the number of diabetics is expected to pass 100 million by 2030. One million die from diabetes each year in India.
Fortunately diabetes is preventable – according to the World Health Organization, 80% of diabetes, 80% heart disease and 40% cancers are preventable with 3 lifestyle changes: avoid tobacco, eat right, and increase physical activity. Now Nalini Saligram could have looked at this as a tell situation. She could have used her background to tell people all the right things that they should be doing. She could have told women that their families’ habits had to change. But this would have fallen on deaf ears because people are resistant to being told what to do. Behavior change is the holy grail of diabetes prevention – it is very difficult to do.
So, she looked for a different approach.
She looked at a multi-pronged community approach, taking prevention to where people live and learn and work.
Arogya World’s Healthy Schools program targets adolescents ages 11 to 14. The comprehensive two-year program includes classroom and school-based activities, as well as outreach in students’ homes and communities. Each year compelling age-appropriate games and learning activities are implemented by trained student leaders or peers. The program’s effectiveness is measured through pre- and post-intervention comparisons of the students’ self-reported knowledge, attitudes and behaviors. Data reported during the first two years of the pilot program (n=2,263) showed an increase in the daily intake of vegetables from 61.2% to 76.9%, 23.7% more students understood that unhealthy eating habits can put you at risk for diabetes, and 66.8% v. 48.9% of students reported that being physically inactive can put one at risk for diabetes. Overall impact on improved health behaviors from the pilot program was estimated to be 14%. Nalini and the Arogya team are now scaling up this program to reach hundreds of thousands of urban and rural school children in partnership with many organizations including Agastya International Foundation and Ashoka’s Nourishing Schools program.
The easiest place to connect with people who are open to ideas and forming their opinions about the world is in schools. Reaching children before their lifestyle habits are set, Nalini believes is smart. But for those that had already passed though the school system, Nalini had to find a different approach. Dragging people back to the classroom was never going to work. Instead she met them in their workplace.
Arogya World targets workplaces for chronic disease prevention because work is where so many people spend a large part of their day. India is a young county with 2/3rds of population under 35 years and the “population pyramid is expected to bulge across the 15-64 age bracket over the next decade, increasing the working age population from approximately 761 million to 869 million during 2011-2020.” [FICCI, EY, 2014]. Many of these employees have sedentary jobs with long, unpredictable hours compounded by long commutes and stress. Arogya World is building an ecosystem of companies in India interested in employee health and wellness.
However the twist is in the way this is accomplished:
Positive news, recognition and encouragement are prime drivers of behavior change, as important as avoidance of pain and suffering. Nalini understands this very well and is pushing the envelope with her “Healthy Workplaces Awards”
Each year in advance of World Diabetes Day, Arogya World holds an annual conference and award event that discusses key issues in workplace health followed by an award ceremony that recognizes the companies for their championship of workplace health. Now in its fifth year, this program and awards attracts the best and biggest employers in India to apply, benchmark themselves and follow through on their commitments to make their environments and their employees’ lifestyle healthier.
The robust criteria that mark a company as healthy were co-created with industry in 2012 to ensure they are viable in the real world: http://arogyaworld.org/healthy-workplaces-criteria/. And these are used by Arogya World in a direct and transparent in-person Assessment process to select the Healthy Workplaces – some 100 companies large and small, spanning >2 million employees in multiple industries in the public and private sectors.
Nalini Saligram thought about the message she wanted to deliver. It had to be engaging and work in a different way to what had gone before. People across the world brush against healthcare advice but don’t pick it up. They sort of understand a little of what is required but don’t pull it together in the form of lifestyle changes. Nalini and Arogya World spoke to people in a ‘sell’ way that made them understand the importance of eating right, but also motivated people to actually go out there and do it. Nalini knows where she is going and has shown proof of concept. To scale up she is looking to make her programs sustainable, work with large partners and expand her community-based approach to prevention in other geographies. We hope she is successful as India’s next generation needs programs like this to stay healthy.
The world of healthcare needs to follow this model. It has many of the elements that we look at in this series on Healthcare Gamechangers
It empowers people to take responsibility of their own healthIt takes the healthcare out of the four walls of the hospital and into the communityIt connects with educators and employers to deliver effective healthcareIt shifts attitudes from illness to wellness and on to healthy living.——-
This post is part of a series on The Healthcare Gamechangers. Read all the stories in this series here.
If you liked this post, you might be interested in my other posts: The Healthcare Gamechangers, Hospitals, a historical perspective and relevance for the future, You are not the Unicorn, You are Awesome, Shoot me if I ever say these things to a startup team, The Doctor is NOT in, the Doctor will see you NOW, and Davos Learnings for my Daugther.
About Ashwin Naik
Ashwin Naik is an entrepreneur with interest in affordable healthcare, social enterprise and healthcare technology. You can also visit his blog to read more.
Ashwin has been recognized as a Economic Times Leaders under 40, Young Global Leader By World Economic Forum, Young Leader by Asia Society, Senior Ashoka Fellow & as a Ted Fellow.
September 27, 2017
Primary care is a team sport
LOOKING AT THE WAY THINGS HAVE BEEN DONE IN THE past only, has limited use for the future. We have worked on models of health for centuries that were right for their time, their technology and the knowledge of the health practitioners. But times have changed significantly. People are suffering from different illnesses now than they were even twenty years ago. The understanding we have as scientists and doctors of complex and obscure parts of the body are far beyond what we could have ever anticipated a short time ago.
Rushika Fernandopulle is one of these visionaries that look at the world for the challenges he can surmount rather than fit in line with the way things are already happening. He co-founded Iora Health and they set out on foundation to challenge the way things were and provide a new way of delivering a sustainable and more effective primary care system.
Their goals were pretty simple –
To improve the service levels given to patients
To provide a better quality of care from the practice
Reduce the expenditure of the healthcare provider
At first glance, these three goals might seem at cross purpose to each other. It is the firmly held belief of many governments, healthcare providers and large portions of the public that to provide better care you need to put more money into the care system. Cutting budgets (as it would be called in a political environment) is a healthcare no-no when it comes to political party manifestos and the way that our politicians court public favor when speaking to their electorate.
IORA HEALTH MODEL
Can you employ non-healthcare workers to provide or deliver majority of the primary care for clients on the phone or in person at their homes?
Turns out, you can.
Iora does this by employing health coaches with customer service background who manage relationships with clients on an ongoing basis, instead of looking at episodes of care and treating just symptoms.
There was a patient who had issues with his health. He had hypertension and type 2 diabetes which went un-managed because of his lack of attention and not enough persuasion from the clinic team in charge of his care. This patient developed renal damage and needed to have dialysis several times every week to deal with this damage. To add to the physical health problems, this patient also suffered from anxieties and would walk out of the 3 to 4 hour dialysis sessions because he just couldn’t cope with what was going on in and around him. So, he would walk away from a scheduled session, return home to feel safe before crashing the next day and being treated with the same dialysis as an inpatient rather than an outpatient. This happened week after week and the patient ended up being admitted 37 times in one year at a cost of several hundred thousand dollars. You can see why this was ineffective for the patient, the medical team and the client base of the practice.
That was until Iora team got involved. As part of their training and guidance they look for alternative solutions to any given situation. With the past giving quite a clear signal in this case of what was going on, the health coach took the time to get to know the patient. They felt this anxiety at home on occasions and in discussion revealed that they counteracted the feeling with music. They listened to music and it made him feel calm again.
With that, the health coach bought an iPod and downloaded music onto it for the patient to use when having the dialysis. The result was that the patient no longer felt anxious at dialysis time, made every appointment, stayed through every appointment and was no longer admitted as an inpatient.
A simple conversation, understanding of the patient’s needs and feelings provided a solution that was more effective than any drug that they were previously given as well as having no side effects and saving the healthcare provider hundreds of thousands of dollars.
Patients often look for the magic bullet. They turn up at a doctor or physician and want to walk away with something physical in their hand that they can take to solve the problem. It is a natural thing to walk in to see a doctor and walk out with a tangible solution. ‘Take one of these three times a day with water after meals.’ It feels like progress is being made.
But the solution is far more often something else. The patient in the example above shows that giving the patient a drug to deal with the anxiety wasn’t working. Maybe it was the patient who initially wanted to see the magic bullet that would solve the anxiety problem. But maybe it was the physician who prescribed it was just following the path of the norm. The normal solution with a patient presenting with symptoms of anxiety is to give them medication that will lessen the effect of the anxiety. Healthcare has got into this rut where we look at problems in terms of prescribed solutions. Every patient is different and feel their symptoms in a different way. The solutions need to be as different and wide ranging as the patients. This takes time initially, with an associated upfront cost, but saves huge amounts of time and money in the long run because, let’s face it, an iPod is a cheaper solution than inpatient emergency dialysis every week or so.
So, how does Rushika Fernandopulle and Iora Health work? They have thrown away the rulebook that states certain symptoms require certain treatments. That doesn’t look at the whole problem and cannot be sustainable in the long term for medicine. Employers providers pay Iora Health to look after patients. They employ a team of healthcare coaches that sit down and actually listen to the patients and what the issues are. The idea is that Iora Health look at the patient in a way that will keep them out of hospital and the specialist office. The iPod example above is a great way of illustrating how this can be done.
The health coaches are selected from a wide variety of backgrounds, the primary criteria being ability to relate to patients and their families. “It’s one of the most innovative models out there. What they’re doing is trying to start to think outside the traditional confines of who can provide care,” said Ashish Jha, a professor of health policy at the Harvard School of Public Health. “You don’t need to go to medical school to be a great health coach, to connect with people and motivate them. Those skills exist much more broadly.”
In the past, the relationship between an employer paying for healthcare and an employee looking to gain treatment have been at odds. The employee wants to try everything they can to get better. More consultations, different opinions and a chance to get better are all in their mind when they walk into a hospital or care provider. They just want to get better, without any consideration for the cost. The doctors end up spending a lot of time trying to persuade the employer that the care is needed and the patient will benefit.
The employer wants a solution, but at the lowest cost possible. They don’t want their employee to go on experimental treatments or to see many doctors for slightly different opinions because there is a large cost involved with this. They want a quick solution that the doctor will find on the first visit. After all, they are paying for all of this.
Iora Health takes a lot of the ‘adversarial’ element out of this situation by looking at the whole person and finding a solution that gets the employee better more quickly, at a lower cost and back to work for the employer. This is the solution that all parties are looking for, but the way that things have always been done means that it isn’t the solution that is most often arrived at. Think about it in terms of pure economics. The healthcare providers of old rely on patients coming back to them for treatment time after time. Iora Health look at this a different way. They charge more than a standard primary care provider to look after the patient for the employer. But they don’t look to have this patient keep doing the same things, costing the same or an increasing amount of money forever more. They look for a way to resolve the situation, or lessen the impact severely so that they can get back on with their life – and the employer that is paying for the treatment gets a happy and healthy employee back on their books as soon as possible. The future isn’t one of prescribing drugs or treatment and following the path that has already been furrowed by others. It is one of managing an illness or condition so it doesn’t affect the daily life of the patient as it had before.
Rushika says the old model does not work at all. The medical industry is full of people who work hard for a living and have the interests of their patients at heart. There is no question about the dedication of the people who work with patients. But the model that they are out into restricts their decisions to a simple choice of treat or not treat. And this decision has to happen fast. There are targets to meet, more patients to see and shareholders to appease. Each medical practice has target times, appointment times and a long queue of people waiting to see the doctor. The pressure on time is immense. The waiting rooms of doctors and hospitals are filled with people who want their magic bullet – and often the patients have busy lives and tight schedules to keep.
The solutions that Rushika Fernandopulle and Iora Health deliver works better for everyone. The medical community get to do what they felt like they were being trained for. They get to deliver healthcare that manages the problems of their patients and allows them to get on with their life.
The patients get a better standard of care. They see the future where their condition or illness has gone or is effectively managed, often by lifestyle changes rather than prescriptions drugs with side effects. They get to feel a little bit better every day and know that they are being listened to.
The people paying for the treatment, in this case employers, get an effective solution that may feel more expensive on day one but is clearly a much more cost-effective way of managing health in the long term. They get employees that know they are being looked after and are more productive in the workplace. In a model where everyone wins, why would we ever look back to an old model that no longer delivers the results that were promised?
Iora Health is a classic example of the Healthcare Gamechangers that i wrote about earlier. Gamechangers who are playing at a higher level by
Making sure everyone plays
The playground is expanded
Invites new players
Changes the rules of the game.
The change won’t happen overnight, but the more we hear of innovative providers like Iora Health, the more likely this solution will become the norm rather than viewed as something alternative. The effective way that patients are treated doesn’t come from looking at targets and crunching more people through the system in an ever-decreasing amount of time. This just isn’t the medicine that you and I know. The long-term answer is to look at the lifestyle of people and make those simple changes early that will keep them out of high-cost care in the years to come. The industry has a lot of work to do in this area.
At the moment, it feels addicted to the way it currently works.
It is an addiction that it needs to be weaned off.
Stay Tuned!
——-
This post is part of a series on The Healthcare Gamechangers. Read all the stories in this series here.
If you liked this post, you might be interested in my other posts: The Healthcare Gamechangers, Hospitals, a historical perspective and relevance for the future, You are not the Unicorn, You are Awesome, Shoot me if I ever say these things to a startup team, The Doctor is NOT in, the Doctor will see you NOW, and Davos Learnings for my Daugther.
About Ashwin Naik
Ashwin Naik is an entrepreneur with interest in affordable healthcare, social enterprise and healthcare technology. You can also visit his blog to read more.
Ashwin has been recognized as a Economic Times Leaders under 40, Young Global Leader By World Economic Forum, Young Leader by Asia Society, Senior Ashoka Fellow & as a Ted Fellow.



