Kathy Brandt's Blog
April 9, 2014
Kathy Brandt and Max Maddox – The Independent Author Network
Kathy Brandt and Max Maddox are the authors of Walks on the Margins, A Story of Bipolar Illness, memoir
via Kathy Brandt and Max Maddox – The Independent Author Network.
April 6, 2014
Mental Health Begins with Me!
Saturday was another big day for mental health care across Colorado. In Colorado Springs more than 200 people joined the second community discussion at the University of Colorado to learn about and make progress on one of the most misunderstood public issues we face today. It’s part of President Obama’s National Dialogue to raise awareness, promote understanding, find solutions, and develop action plans to address the who live with mental illness.

Jason DeaBueno
Jason DeaBueno, vice-president of AspenPointe, a local non-profit that provides mental health services, spoke hopefully about our progress.
The new Health Care Act, he said, is helping people who previously depended on emergency rooms “to find their way to care.” That, along with Governor Hickenlooper’s recent initiatives to develop more mental health centers means more access for those who need it. But there is still much to do and engaging the community in solutions is critical.

Make Change Happen!
DeaBueno urged each of us step up on our soapboxes’ and speak out for change.
March 20, 2014
A Poem about Bipolar Disorder & Stigma
A Poem about Bipolar Disorder & Stigma by Joye Chizak
The Last American Outcast
So I went to the Smithsonian
and sought out the lunch counter
taken from the Woolworth’s in Birmingham
some fifty years ago.
Slipping under the velvet rope
I pick the pink leatherette stool on the end
and wait to be served.
All these weirdos
the stench of outcasts still lingering in the air
catsup hemorrhaged like blood thickened by the musk of history,
me, the last of them
here
right in their spectral midst.
I had never known nor ever even imagined
for a heartbeat
that it would come down to a person like me.
The curator is called
and comes clicking swiftly perplexed.
“You are in a restricted area. What do you want?” she says in a stage whisper.
“To be served…like the others”, I say.
“But you ‘re not even black…” she pleads quietly.
“No, and I am not Irish or Muslin or Lesbian …they all would be served.”
“Who are you? What do you want?”
“ Just a stuffed tomato with chicken salad …and perhaps an ice tea, no lemon.”
“ Who are you?” she asked again,
cocking her head like a chicken looking for defects unseen to her naked eyes.
“I’m a mentally ill American. “
Her eyes widen and she speaks quickly into her phone calling for back-ups.
“I have legal rights. You cannot discriminate”,
by then, suited men pick me effortlessly off the sacred pink artifact and carry me away.
I glance back at the ghosts,
eating grilled cheese sandwiches and sipping cokes
clinking glasses together…the Jews, Gays and Latinos.
My time has not yet come.
The last outcast in America,
not welcome at the great lunch counter of this free and accepting land.
About Joye Chizak:
Joye was diagnosed with bipolar disorder in 1980 and has been stable on lithium since 1982. She worked professionally in marketing, now runs her own consulting firm in 2000. She remembers the time she worked briefly at a regional chamber of commerce with young people and disclosed her bipolar illness. Subsequently she was cut-off from executive communication and her duties were downgraded despite her tangible achievements. She’s been writing about the Last American Outcast ever since and also written a short, illustrated book for the loved ones of those with bipolar called Bipolar Bootcamp.
March 12, 2014
What Does it Feel Like to Live With Bipolar Illness?

Writing Heals
I’ve started this Q&A about bipolar disorder as a way to engage those with bipolar illness and their families in telling their stories. Perhaps by reading others stories, you won’t feel so alone. And writing about your personal exoeriences helps other and it can help you because writing heals. Please join our conversation.
To get you started–A question for those who have bipolar illness, one for families, and one for spouses and significant others. Feel free to go wherever your writing takes you:
Q: What does it feel like to have bipolar disorder? Have you found any strategies that make life easier?
Q: What is it like to have a family member with bipolar disorder? Have you found strategies to cope?
Q: What is it like to have a spouse or partner with bipolar disorder? What difficulties have you had in maintaining the relationship ?
Here’s my story as a mom:
Difficult but Heartfelt
“My son was 20 and beginning his junior year in college when he had his first episode. After that Max had an episode every year. He disappeared among the big city homeless, ended up handcuffed in the back of police cruisers, and came within inches of jumping from a shattered eighth floor window in Philadelphia. By the time he was twenty-six, he’d earned a dozen commitments to psychiatric institutions.
For me the homeless pushing grocery carts filled with their meager belongings became encounters too close to home. I struggled to come to terms with my changing role as parent and confidant. Stymied, bullied, blindsided by doctors, hospitals, and the law, I chased Max’s collapsing dreams and I was afraid he wouldn’t live through the next crisis.
I’ve spent hundreds of hours in psychotic hospitals. Over the years I’ve learned how horribly inadequate our mental health care “system” is. Finding good treatment for Max was more than just difficult—it was often impossible. Patients and families are dictated to, appointments with doctors are hard to come by, those in crisis end up in emergency rooms where they wait for help that never comes, outpatient care is practically non-existent, and too many psych units are simply holding tanks, places where little treatment occurs except for the piling on of medication. Already severely traumatized from his illness, Max has been restrained, isolated, and physically abused by staff that are undertrained or just don’t care. Needless to say, it broke my heart.
After one lengthy hospitalization, l was told that Max would never recover. “Max can’t live on his own,” the doctor said. “You better plan for the future. You’d better. You’d better. You’d better.” The message—you’d better give up hope. I had to reject the hopelessness that doctor tried to hand me because the alternative was simply too devastating. I was angrier than I’d ever been, angry at a mental health care system that had failed us so completely and at that doctor.
To cope I finally found NAMI (National Alliance on Mental Illness), where got educated, found enormous support from other parents, and became an advocate for my son and others. Other coping mechanisms included yoga, meditation, and time with grandchildren. In these sweet beings there is nothing, if not hope.
Most important, I’ve learned that people with mental illness can and do succeed. They live fulfilled lives, working in jobs, volunteering, and developing significant relationships. They engage in the process of recovery, knowing that recovery doesn’t mean cure. How do they do it? They believe in themselves. They persevere through hardship. They risk failure. They define their own life goals and design their unique paths based on their own limitations, needs, strengths, preferences, and backgrounds. They are supported by allies—family, friends, peers, who believe in their potential to be their best, who stand by them, offering hope, and support.
As part of coping and healing, Max and I eventually wrote a book together about our journey. Reliving the years of trauma was painful for both of us, but ultimately it helped us make sense of all the chaos. And something about the writing makes the pain less intense. It was a risky venture, especially for Max, who has brought his illness into the light for everyone to see. But it has felt like the ultimate step in recovery for both of us.” —Kathy
Thank you to these two friends for writing about their bipolar illnesses:
“When I was diagnosed with bipolar disorder around six years ago, I had long been aware that my brain was somehow oriented in a different direction than anyone else’s brain I knew of. Receiving a diagnosis only put a name on an experience I was already familiar with. Six years later, I have no distinct conclusions, no cures, no answers about bipolar disorder. I can only describe my  personal experience, and I do so in an attempt to better understand how to function despite my struggles. I often regret who I was and what I did while in manic states, or the time that got wasted during months of depression. I’m working on my relationship to my memories. I don’t know how to treat them, interact with them, or understand them. I think I need to accept the past as something that I experienced, and that’s it. But I want to turn and run away from my memories, I cringe at the thought of them. So instead, I try to focus on where I am now – A stable, healthy place that took a great deal of hard work to reach. Of course, this does not mean I no longer struggle. My medication helps me manage, but there are always weeks when it is impossible to get out of bed. I engage in a constant battle with anxiety, which I can only describe as being perpetually stuck in the moment between tripping over something and landing on the pavement. Severe anxiety feels like being frozen in this moment, forever trying to hold myself in the position that will hurt the least when I inevitably hit the ground. In my experience, bipolar disorder means knowing how and when to ask the people who love you for help. It means accepting the mistakes you made, the delusions you had, and the damage you caused. It requires a great deal of self-awareness, patience, and forgiveness. These are not things I’ve mastered yet, but as time goes on, I gain greater insight into how bipolar has controlled me, and what I need to do in order to regain that control. Mental illness is not charming, “quirky”, or temporary. It is a huge weight that I anticipate carrying for the rest of my life. The trick is not figuring out how to cast off this weight, but rather to acknowledge its presence, get a firm grip around it, and carry on.”–Anonymous
personal experience, and I do so in an attempt to better understand how to function despite my struggles. I often regret who I was and what I did while in manic states, or the time that got wasted during months of depression. I’m working on my relationship to my memories. I don’t know how to treat them, interact with them, or understand them. I think I need to accept the past as something that I experienced, and that’s it. But I want to turn and run away from my memories, I cringe at the thought of them. So instead, I try to focus on where I am now – A stable, healthy place that took a great deal of hard work to reach. Of course, this does not mean I no longer struggle. My medication helps me manage, but there are always weeks when it is impossible to get out of bed. I engage in a constant battle with anxiety, which I can only describe as being perpetually stuck in the moment between tripping over something and landing on the pavement. Severe anxiety feels like being frozen in this moment, forever trying to hold myself in the position that will hurt the least when I inevitably hit the ground. In my experience, bipolar disorder means knowing how and when to ask the people who love you for help. It means accepting the mistakes you made, the delusions you had, and the damage you caused. It requires a great deal of self-awareness, patience, and forgiveness. These are not things I’ve mastered yet, but as time goes on, I gain greater insight into how bipolar has controlled me, and what I need to do in order to regain that control. Mental illness is not charming, “quirky”, or temporary. It is a huge weight that I anticipate carrying for the rest of my life. The trick is not figuring out how to cast off this weight, but rather to acknowledge its presence, get a firm grip around it, and carry on.”–Anonymous

You Are Not Alone
“It’s a struggle because everything a doctor can do for you feels like guesswork and the medication can be almost as bad as the disorder itself. It’s pretty alienating sometimes and it can be really extremely hard to have any real objectivity about the world around you are always struggling internally. I just finally have found a medication combination that actually does anything and even now its hard work all the time. It also can be really revealing in terms of figuring out the nature of your interpersonal relationships. Fair weather friends will more than likely leave and you end up left with the people who are really capable of understanding you and being supportive in a real and ongoing way.
I do a lot of breathing exercises because I have sort of co-morbid anxiety. Really the most important thing is to push myself to do the things that feel impossible. Sometimes that’s just like going out with friends when it feels completely counterintuitive. Honestly I genuinely believe in faking it until you make it. As long as you acknowledge your feelings it’s important to try to keep a semblance of normality. It’s also important to be honest with the people around you. I see a psychiatrist and a therapist once a week. I also have scheduled hours for sleep and for exercise because having a schedule makes a huge difference.” –Anonymous
I hope you will join us in sharing your story. With every best wishfor healing and recovery.
March 7, 2014
Community Conversation Takes on the Stigma of Mental Illness
Patrice Winsor was one of five panelists kicking off community dialogue in Colorado Springs last night. Patrice, who lives with bipolar disorder and ADD, said her healing began while talking about her struggle with fellow teens. Up until then, she didn’t realize that others battled similar issues. The point? We  need to talk about mental illness in spite of the stigma that surrounds it. And that’s what happened in Packard Hall at Colorado College as 230 people came together to talk about the state of mental health in the region and how to fill the gaps in care. I was thrilled to be among them and participating in a conversation that means so much to me as a mother who struggled over the years to find help for my son.
need to talk about mental illness in spite of the stigma that surrounds it. And that’s what happened in Packard Hall at Colorado College as 230 people came together to talk about the state of mental health in the region and how to fill the gaps in care. I was thrilled to be among them and participating in a conversation that means so much to me as a mother who struggled over the years to find help for my son.
Discussion centered on the lack of education and awareness of mental illness in the community, the toll mental illness takes on families, the effects on business, the costs to society, and more. After the panel discussion, small group dialogues began. No one was reticent to share their experiences and passions about the issues.
This was the first of three forums scheduled over the next months. The goal? To prioritize and develop community-based solutions and localized health action plans by June, 2014 and to implement them with a statewide fundraiser.
As I left the session, I was reminded that “a small group of thoughtful, committed citizens can change the world; indeed, it’s the only thing that ever has.”
January 29, 2014
Looking for Hope in a Guide to Bipolar Disorder
The glass doors caught my suitcase as I stepped into a hollow lobby and got onto the elevator, surrounded by doctors in scrubs and baggy-eyed visitors with paper coffee cups in their hands. One by one they stepped off at their appointed floor—cardiology, pediatrics, oncology. On seven, signs to “Psychiatric” led me to a steel door with a tiny  window webbed with fine metal strands.
window webbed with fine metal strands.
“You have to leave your suitcase and purse and anything you’ve brought for Max here. We’ve got to check everything. No sharps,” which I learned included belts, nail clippers, pens, even the half-filled bottle of juice I had tucked under my arm.
I found Max lying in his bed, legs drawn up to his chest. “Matty,” I whispered. He sat up and smiled—looking at me with a haunted kind of relief. I wrapped my arms around him, thankful to have my hands on my kid, his frame angular and sharp. His eyes retreated into hollow orbs above edged cheekbones; his body slouched with exhaustion. Ugly torn blisters, red and bleeding, covered his heels and toes. He turned onto his belly and I kneaded his shoulders, ran the heel of my hand along each side of his spine. He was so quiet and I wondered where his mind drifted. I had no inkling of what he was experiencing—whether he was glad or scared, reliving his days on the streets of Chicago, or lost somewhere else entirely.
I spent hours in the psychiatric unit that week, interrupted only by walks along Lake Michigan or wanderings through the Water Tower, a vertical mall just blocks from my hotel. I often ended up in the bookstore, sitting on a stepstool with yet another book about bipolar disorder open in my lap. I studied the pages, eighty on medication alone: SSRI’s, MAOI’s, Benzodiazepines, anti-psychotics, calcium channel blockers, and drug complications. Somewhere in these pages, I hoped I’d find answers from the experts. But their advice was thin. I needed something more immediate.
So I began my own list:
#1—Try to smile when you walk onto the psych unit.
#2—Remember that normal is overrated.
#3—Don’t give up the battle with the insurance company and their message machines.
#4—Control yourself when the doctor who says he’s always in by seven doesn’t show up until you decide to go get lunch and is gone by the time you get back.
#5—Never cry in front of Max.
#6—Call your sister and cry to her instead.
#7—Remember to eat and sleep.
#8—Pretend you’re not afraid.
#9—Know that Max and I will get through this.
#10—When things seem hopeless, reread the sentence in the book that says, “Winston Churchill had manic depression.
Excerpted from “Walks on the Margins: A Story of Bipolar Illness”
Looking for Salvation in a Bipolar Guide
Looking for Salvation in a Bipolar Guide
(An excerpt from Kathy and Max’s memoir, Walks on the Margins: A Story of Bipolar Illness)
The glass doors caught my suitcase as I stepped into a hollow lobby and got onto the elevator, surrounded by doctors in scrubs and baggy-eyed visitors with paper coffee cups in their hands. One by one they stepped off at their appointed floor—cardiology, pediatrics, oncology. On seven, signs to “Psychiatric” led me to a steel door with a tiny window webbed with fine metal strands.
“You have to leave your suitcase and purse and anything you’ve brought for Max here. We’ve got to check everything. No sharps,” which I learned included belts, nail clippers, pens, even the half-filled bottle of juice I had tucked under my arm.
I found Max lying in his bed, legs drawn up to his chest. “Matty,” I whispered. He sat up and smiled—looking at me with a haunted kind of relief. I wrapped my arms around him, thankful to have my hands on my kid, his frame angular and sharp. His eyes retreated into hollow orbs above edged cheekbones; his body slouched with exhaustion. Ugly torn blisters, red and bleeding, covered his heels and toes. He turned onto his belly and I kneaded his shoulders, ran the heel of my hand along each side of his spine. He was so quiet and I wondered where his mind drifted. I had no inkling of what he was experiencing—whether he was glad or scared, reliving his days on the streets of Chicago, or lost somewhere else entirely.
I spent hours in the psychiatric unit that week, interrupted only by walks along Lake Michigan or wanderings through the Water Tower, a vertical mall just blocks from my hotel. I often ended up in the bookstore, sitting on a stepstool with yet another book about bipolar disorder open in my lap. I studied the pages, eighty on medication alone: SSRI’s, MAOI’s, Benzodiazepines, anti-psychotics, calcium channel blockers, and drug complications. Somewhere in these pages, I hoped I’d find answers from the experts. But their advice was thin. I needed something more immediate.
So I began my own list:
#1—Try to smile when you walk onto the psych unit.
#2—Remember that normal is overrated.
#3—Don’t give up the battle with the insurance company and their message machines.
#4—Control yourself when the doctor who says he’s always in by seven doesn’t show up until you decide to go get lunch and is gone by the time you get back.
#5—Never cry in front of Max.
#6—Call your sister and cry to her instead.
#7—Remember to eat and sleep.
#8—Pretend you’re not afraid.
#9—Know that Max and I will get through this.
#10—When things seem hopeless, reread the sentence in the book that says, “Winston Churchill had manic depression.”
January 16, 2014
Kelly Thomas: Schizophrenic & Disposable
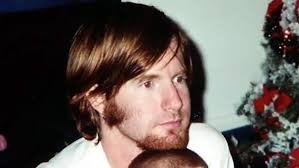
Kelly Thomas
This week, a jury acquitted Fullerton, California, police officers of any wrong doing inthe beating death of Kelly Thomas, who was thirty-seven and suffering from schizophrenia. I watched the surveillance video of the beating, which was also shown in court. Kelly’s parents saw it too. It was horrible, tragic, heart-breaking and unnecessary. On moment Kelly is sitting on bench, perhaps talking to himself, maybe hearing voices, the next a police officer appears pulling on latex gloves and looking like he’s ready to enter the ring. The match is pretty one sided though. “Sorry, sorry, I can’t breathe, man. Sorry,” Kelly yells as he is repeatedly kicked, tasered, and beaten beyond recognition. He cries out “Dad, Dad. Help me Dad. I love you Dad.” After five days in a coma, Kelly Thomas died.
How could officers beat a man to death for no apparent reason and how could the jury conclude that it was okay? The defense attorney argued that Kelly was combative, but when I looked at that video, I only saw a man fighting for his life. Why didn’t the jury see what I saw? Are the mentally ill so undeserving and so easily disposable? Was Kelly Thomas to be blamed for his illness? Were his parents to blame for letting him roam the streets? Many seem to think so. Utter nonsense. Kelly Thomas was on the streets because we don’t have a system of care that ensures treatment to those who need it, including commitment to a hospital. Seemingly Kelly Thomas wasn’t “a danger to himself or others,” the criteria for commitment in most states. And as an adult he had the “right” to be unmedicated and homeless. I’ve seen it many times before— parents powerless to get the help they so desperately want for their son because of the laws and inaccessibility of treatment. So the police are left to deal with it and too often those with mental illness end up dead.

Kelly Thomas Never Regained Consciousness
Unfortunately, instead of mental health professionals, it is the police who are on the front lines when it comes to those with mental illness. They deal with scores of mental health crises every day because of our failed system. They have become our defacto mental health care providers and they are ill-equipped to fill that role. Even so, many officers do what little they can to help them. They transport them to emergency rooms and crisis centers, only to see those same faces back on the streets a day or two later.
One attempt to educate those officers who must deal with psychiatric emergencies is Crisis Intervention Training (CIT), a program supported by NAMI (National Alliance for Mental Illness). Officers who complete the training say their attitudes toward those with mental illness are transformed. They are educated about what it’s like to live with severe illness and learn to empathize with those who suffer. They learn how to respond to crisis with understanding and compassion and to de-escalate situations. Many communities have instituted CIT after tragedies such as that of Kelly Thomas. Fullerton needs to do the same. And as a country, we need to change our perceptions about mental illness and treat it as an illness like any other.
January 15, 2014
When Someone You Love Lives with Severe Mental Illness
Today I’m pleased to welcome Tamara Hill, MS, as my guest writer. Tamara is a therapist specializing in child and adolescent mental health. Although she has worked with trauma and autism spectrum disorders, she gleans most of her experience from working with parents, families, and caregivers within the mental health system. She is well known for her advocacy and has spoken on a variety of radio shows, both nationally and internationally, and contributes to multiple media outlets. As a family consultant and advocate,
 Támara aims to empower families to re-discover authentic living outside of a complex and unfair system.
Támara aims to empower families to re-discover authentic living outside of a complex and unfair system.
Severe Mental Illness: Self-Knowledge Makes All The Difference
By Tamara Hill
Do you have a loved one suffering from a mental health condition? Is it mild, moderate, or severe? Can your loved one function independently without you and if not, what are your thoughts about this? These questions were posed to an audience of parents, families, and caregivers at a NAMI parent-to-parent and family-to-family meeting I attended back in April of 2013. I sat amongst a group of mothers, aunts, and siblings who were drastically affected by the mental health condition of their loved one. These families had been exposed to the horrifying consequences of untreated and poorly treated mental illness such as homelessness, incarceration for petty offenses (some major), victimization (rape, murder, robbery), and violence. As I listened to the families share their stories and ask questions, I observed all of us communicating in almost a frantic manner. It was like I stepped outside of myself and could see that we were all so very similar in our plea for change. We recognize that society is becoming the victim of a larger system that criminalizes, ignores, and devalues families almost everywhere. As a therapist, I feel responsible for speaking out on this topic and using my knowledge to educate families. As a friend to someone I love dearly who is suffering, I feel motivated to de-criminalize the innocent victims of poor mental health and impulsive decision making. My career has become my life’s calling, my passion, my responsibility.
After such an earthshattering revelation, I got to work. I found major problems in the system, but currently focus on 3 major issues:
1. Parents, families, and caregivers are highly devalued in the mental health system: Unfortunately, many parents and families are put on the back burner if their child is 14-years-old and older in many states. In PA, for example, a 14 year old can reject treatment and keep certain details hidden from their families. Mental Health Professionals are at no obligation to share “non-threatening” details with a family. In many cases, talk of suicide or homicide may or may not reach the ears of a family if a professional determines it unnecessary. If a 14-year-old requires medication, this too will not include parents and family. This is too much power in the hands of youngsters and strangers (i.e.., mental health professionals).
2. Civil commitment laws have created more tragedies than society is aware of: Civil commitment laws prevent families from having a “dangerous” or self-injurious loved one committed for their safety and the safety of others. In moments of great distress, families are left alone to determine the best options for their loved ones. In many cases, there are few options available to families because of the law. The law prevents appropriate and timely treatment.
3. Lack of support and resources for families experiencing a crisis: A family is often left alone to make decisions on their own. Families who are uninformed about the system operate on trial and error, asking multiple questions during short encounters with healthcare professionals, or reading multiple books from a library. Research on the Internet, asking friends and co-workers, or making multiple mistakes is often how parents and families get by. This should never be!
Self-knowledge is extremely important for parents, families, and caregivers. Because families are often on their own to figure things out, there are 2 important things I encourage you to do if you have a suffering loved one:
Engage in psychological preparation.
1. Accept that you can encounter a crisis or emergency any day, any time: Acceptance of reality makes the reality you may have to face, a tad easier.
2. Have a plan: Write down, in a notebook dedicated to your “crisis plan,” things you could do if an emergency occurs. For example, if your loved one begins to hallucinate, write down what your first few steps might be. Will it be a discussion with your loved one? Will it be hospitalization? Will you enlist the help of family or friends? Also consider if calling the police would make matters worse or better.
3. Engage in self-care: Helping yourself before you can help someone else is extremely important. Resting your mind, taking breaks, and caring for yourself is almost like preparation for the unknown.
Engage in behavioral preparation.
1. Know what you will do and say: When emergencies occur, it’s really easy to say and do whatever comes to mind. I’m guilty of this myself! But you want to have some idea of what you will do. Speaking calmly is often helpful, calling others for help, having emergency numbers close, etc. are all helpful. I often encourage families to keep emergency numbers on them at all times and memorize them if you can.
2. Know how you will subdue threatening behavior: In cases of severe mental illness where violence is a possibility, be vigilant and know what you will do if your loved one’s behavior becomes violent or self-harming. It’s difficult for people to associate violence with those they love, but an illness often removes your loved one from reality, increasing the possibility of violence. Have a plan.
Coping with a loved one’s condition can be very stressful for everyone involved. It is emotionally, psychologically, and physically overwhelming. This is why I encourage self-care, creating a crisis plan, and teaming up with people who can support you. Gain as much self-knowledge as you can. We live in an “every man for himself society” and sadly, that mentality circulates throughout our mental health system. But you can guard against this by knowing how to protect yourself and those you love.
I wish you well.
December 4, 2013
Antipsychotics Revisited
Back in July, I wrote a blog here and an article for Mad in America titled “
Case Against Excessive Use of Antipsychotics”  about Robert Whitaker’s lecture at the NAMI Convention that my son Max Maddox and I attended. In the blog I talked about how shocked and confused we and others in the audience were about Whitaker’s argument that antipsychotics could cause more harm than good and that they should be used selectively and perhaps not at all. The response to that blog was overwhelming, with people from all sides of the argument weighing in—not just about antipsychotics, but about alternative treatments, how we talk about the experiences of psychosis, the use of the term “illness,” and the financial interest of drug companies that are making billions from these drugs. There were stories from people who said that their medication saved them and from those who said going off them returned them to the self they had once been. Many said that we each need to make our own choices based on what works for us and I certainly agree. There is no cookie cutter approach. But we need accurate information to make the right decisions. That can be hard to come by in a climate that has become so politicized and polarized.
about Robert Whitaker’s lecture at the NAMI Convention that my son Max Maddox and I attended. In the blog I talked about how shocked and confused we and others in the audience were about Whitaker’s argument that antipsychotics could cause more harm than good and that they should be used selectively and perhaps not at all. The response to that blog was overwhelming, with people from all sides of the argument weighing in—not just about antipsychotics, but about alternative treatments, how we talk about the experiences of psychosis, the use of the term “illness,” and the financial interest of drug companies that are making billions from these drugs. There were stories from people who said that their medication saved them and from those who said going off them returned them to the self they had once been. Many said that we each need to make our own choices based on what works for us and I certainly agree. There is no cookie cutter approach. But we need accurate information to make the right decisions. That can be hard to come by in a climate that has become so politicized and polarized.
But there is what we might consider good news. In terms of the issue of anti-psychotics, it seems important factions are reaching some consensus. In August NIMH director Thomas Insel wrote that “results from several studies have suggested that these medications (antipsychotics) may be less effective for the outcomes that matter most to people with serious mental illness: a full return to well-being and a productive place in society.” Some called it a victory for mental health reformist. I prefer to think of it as a victory for those of us in the trenches of illness who want to make informed choices.
 But I can only imagine how those who have been on antipsychotics for years and their families feel about such findings which also indicate that antipsychotic medications cause brain damage and worsen prospects for recovery over the long-term, and how they feel when they learn that studies by NIMH and APA thirty-six years ago (1977) were indicating that antipsychotics weren’t the miracle medication some believed.
But I can only imagine how those who have been on antipsychotics for years and their families feel about such findings which also indicate that antipsychotic medications cause brain damage and worsen prospects for recovery over the long-term, and how they feel when they learn that studies by NIMH and APA thirty-six years ago (1977) were indicating that antipsychotics weren’t the miracle medication some believed.
So what are those who develop schizophrenia and psychosis to do? In 2009, NIMH began a research study called RAISE ( Recovery after initial schizophrenic episode Initiative) which calls for intervening immediately upon first diagnosis, systematically incorporating options include medications, psychosocial treatments, and rehabilitation, including teaching patients and families how to manage the disease. According to Insel testing is being conducted in community health centers in 23 states. http://www.nimh.nih.gov/about/director/2013/network-solutions.shtml. Hopefully it won’t take thirty-six years to determine the effectiveness.
In addition, much is being written about Open Dialogue, begun in Finland by Jaako Seikkula. It requires early intervention and family and community-based therapy that involves dialogue with patients and the people most affected by their mental health crises. Seikula recommends intervention within days of psychotic onset. Training for the program is now offered in the US by Mary Olsen of the University of Massachusetts at The Institute for Dialogic Practice in Massachusetts. Recent, the Vermont Department of Mental Health awarded a $15,000 grant to Burlington Howard Center for a pilot project — the first of its kind in Vermont — that will train staff in Open Dialogue. Medications aren’t ruled out but are not a focus for treatment. Though success rates are promising, further investigation needs to take place.
But what are those who have been on antipsychotics for years and who are chronically and severely ill to do? Certainly neither Open Dialogue nor RAISE are options. What does good treatment look like for them, and where are they to go to get it? Do they remain on their antipsychotics and simply stay the course? Is it possible for them to taper off and will doing so restore them to well-being and a productive place in the community or shatter them completely?
Fortunately Max has never been on antipsychotics for an extended time. After I wrote that first blog, many emailed to ask what he is doing about medication and how he’s doing. To find out. visit his blog: www.walksonthemargins.com




