Patsy Catsos's Blog
March 24, 2025
How Can I Get Enough Fiber on a Low-FODMAP Diet?
A. Low-FODMAP diet does not equal low-fiber diet. Low-FODMAP servings of fruit, vegetables, beans, lentils, nuts, seeds and whole grains can (and should) be part of your low-FODMAP diet to help you get enough fiber. Keep the low-FODMAP phase of the diet short, so you can eat your favorite high fiber foods again as tolerated later on in the FODMAP elimination diet process.
What is fiber?
Beautiful, tasty, and low-FODMAP food sources of fiber: a wedge of squash with skin, stuffed with quinoa and garnished with pecans.
Fibers are certain types of carbohydrate found in plant foods. The building blocks of fiber are sugars, linked together like a chain. Those links cannot be broken down by digestive enzymes; that is actually part of what defines them as fibers. Fibers stay in the gut, where they are an important source of food for the normal gut microbiome. The gut microbiome is the community of bacteria and other microbes present in your large intestine (colon). Fibers that feed the good bacteria in your gut microbiome are called prebiotics.
I like to use the word fibers whenever I can, with a “s” on the end—fibers are not just one thing. There are many different types of fibers found in food, and they all have a role to play in good health. There are many ways to describe fibers, but the characteristic that determines which fibers are FODMAPs is the “chain length”, in other words the number of sugar molecules linked together.
O is for oligosaccharides.In the FODMAP acronyms, O is for oligosaccharides, which means “short chains sugars”. Two very short chains sugars, fructans (chains of fructose) and GOS (chains of galactose), fall under the FODMAP umbrella. Biochemists might described them as sugars, but functionally they are fibers (they are carbohydrates that cannot be broken down by digestive enzymes).
F is for (Rapidly) FermentableFructans and GOS, being very short chains of sugars, are small molecules. Small molecules have a very high surface area compared to their volume. Bacteria can quickly eat their way around and through them, rapidly producing gas, which results in uncomfortable symptoms for people with IBS if we eat too much of them at one time. Only the most rapidly fermentable fibers are FODMAPs. Longer-chain fibers are fermented slowly enough to cause less trouble with excess gas and bloating and they are good food sources for a healthy gut microbiome. Resistant starches are other well-tolerated prebiotic substances in food that are technically fibers. When starchy foods like rice, potatoes, oatmeal, and cornmeal are cooked and cooled, the starch molecules in them change to forms that resist digestion. These resistant starches serve as food for the gut bacteria, but due to their tremendous molecular size, they are only slowly fermented.
Too much of a good thing?Fibers are good for you. In addition to serving as prebiotics, fibers are filling, helps maintain healthy blood sugar and cholesterol, and help us have formed, regular bowel movements. But too much of a good thing can cause miserable gastrointestinal symptoms for many people with IBS. The FODMAP elimination diet will help you learn your limits. Even on the low-FODMAP phase of the diet, do the best you can to eat food sources of fibers at every meal, using the strategies below. (For the record, 20-35 grams of fiber daily would be nice to aspire to.)
Don’t be an over-achieverDo NOT just stop eating high fiber foods that have small low FODMAP serving sizes. I meet too many people that just stop eating beans and fruits and vegetables on their low FODMAP diets. You’ll only be hurting your nutrition and your food quality of life if you try to eat no FODMAP fibers at all.

Add some chickpeas or beans to your low-FODMAP salad to get more fiber!
Choose 2-3 low-FODMAP servings of fruit, and 3-4 low FODMAP servings of vegetables every day. Eat them unpeeled for extra fiber.
Choose 1-2 low-FODMAP servings of nuts or seeds every day. Add 2 tablespoons of walnuts or pecans to your salad, or snack on peanuts. Chia and flax seeds taste good in oatmeal and smoothies.
Choose whole grains at each meal, such as oatmeal, brown rice, quinoa, or whole-wheat sourdough bread.
Add 2-3 tablespoons of beans or lentils to your soup or salad.
Fiber as a food ingredientGet your fiber from the whole foods suggested above. I don't recommend processed foods with most types of added, isolated food fibers for people with IBS who are following low-FODMAP diets. These are common causes of IBS symptoms. Examples of these isolated food fibers to avoid are inulin, chicory root, chicory root extract, beet fiber, soy fiber, and other industrial fiber ingredients that are added to food to boost the fiber content. Bars, gluten-free baked goods, breakfast cereals, protein powders and shake mies often have added fibers because they would be otherwise poor fiber sources. If the front of the package says, "high fiber!" or “low net carbs”, be sure to read the fine print of the ingredients section.
Fiber supplementsWhat about fiber supplements? I generally discourage changing, stopping or starting fiber supplements during the elimination diet process. Sometimes, if constipation doesn’t improve as much as hoped on the first few weeks of the elimination phase, it is helpful to add one. In that case, I tend to recommend those made of psyllium husk, starting with a very small serving and increasing slowly over time. Other good candidates are acacia gum or fiber and partially hydrolyzed guar gum. Avoid fiber supplements made of inulin, which is an out-and-out FODMAP.
Originally published June 4, 2014. Updated in 2020, and again more recently on March 24, 2025.
This page may contain affiliate links. We are a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
January 16, 2025
How can I get enough calcium on a low FODMAP diet?
A. There are plenty of good sources of calcium on a low-FODMAP diet if you consume dairy products. If you avoid dairy for some non-FODMAP reason, you may not be able to achieve the recommended level of calcium intake without a supplement.
Calcium ReQuirementsCalcium is a mineral, and an essential building block for strong bones. Most of the calcium in your body is stored in your bones. Calcium also circulate in your blood, where it plays critical roles in muscle contraction, nerve signaling and blood clotting. The calcium level in your blood must therefore be very stable. Calcium is drawn from your bones when there isn’t enough calcium in your diet to maintain normal blood levels. Bone is living tissue that is continually being broken down and built back up. Osteoporosis occurs when the creation of new bone tissue doesn’t keep up with the loss of old bone. The bone mineral density of osteoporotic bones is low. Osteopenia is an early sign or stage of osteoporosis.
Your calcium needs depend on your age and sex. In the U.S. and Canada, recommended intakes are the same whether your bone density is normal or in the osteopenic or osteoporotic range. Adults up to age 50 should consume 1000 milligrams (mg) of calcium per day from a combination of food and supplements. Recommended intakes increase to 1200mg at age 51 for women and at age 70 for men. (Pre-teens and teenagers need more calcium, 1300mg per day.) Health authorities in some countries set lower targets for calcium intake. In the U.K, guidelines recommend intake of 700mg for most adults (1000mg for people on osteoporosis drug treatment), which might give you some comfort if you’re not able to achieve a higher intake.
What if I Don’t eat dairy? Can't I get the nutrients I need from other foods?There is little chance of getting 1200mg of calcium per day from non-dairy foods unless you are committed to eating 1-3 servings of tofu daily along with small bone-in fish, tiny shell-on shrimps, and loads of greens, as many do in traditional Asian diets. Two full cups of fortified almond or rice milk every day would go a long way toward meeting your needs, but who does that? Most people choosing a dairy-free diet will need calcium supplements to meet their needs.
Good Low FODMAP Calcium sourcesThese foods are among the strongest sources of calcium in the low-FODMAP serving sizes suggested in the Monash FODMAP Diet App:

Firm tofu, as opposed to silken tofu, is a source of calcium because it is made with the naturally occurring coagulant calcium sulfate.
Lactose-free milk (300mg), lactose-free yogurt (180-290mg), lactose-free kefir (325mg), Cheddar cheese (300mg). sardines (400mg), calcium-fortified almond or rice milk (300-450mg), tofu (500mg), canned salmon, with bones (240mg), chia seeds (150mg), bok choi (75mg), corn tortillas (150mg), and sourdough bread (66mg).
The calcium from most other low FODMAP foods just doesn’t add up very fast. This can be due to the limited serving sizes, or because they just aren’t as rich in calcium as you may think. For example, the low-FODMAP serving size of kale, 1/2 cup raw, contributes just 12mg of calcium. Three-fourths (3/4) cup of broccoli has 30mg of calcium, one tenth the amount in a serving of yogurt. Low FODMAP servings of canned legumes (20mg) or almonds (30mg) are other minor contributors.
Label reading for calcium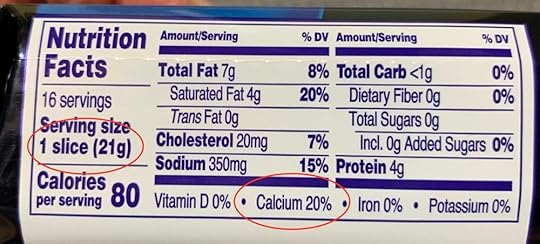
The Daily Value (DV) for calcium is 1300mg. One serving of this food contains 20% of the DV, or 260mg (.20×1300=260).
Sometimes the Nutrition Facts panel spells out the amount of calcium in a serving of packaged food. In other cases you have to calculate it yourself, especially on small packages of food with limited space for details. Pay close attention to the serving size shown vs. the amount you actually eat or drink, and do the necessary math to calculate your intake. For example, a cup of lactose-free milk might well contain 300mg of calcium, but if you only put 1/8 cup of milk in your tea, you’ll be getting 37.5mg. (300÷8=37.5).
The target amount of nutrients used as a reference on Nutrition Fact panels is called the Daily Value, or DV. Why is the DV for calcium 1300mg? The DVs are not specific to any one age or gender. In this case, the reference amount of calcium selected for use as the DV was the higher amount recommended for older children and teens, rather than the 1000mg or 1200mg for adults.
Some foods don’t have Nutrition Facts panels, such as fresh fruits and vegetables. Sometimes you get lucky, and Google will present good quality data prominently on the page when it returns results for queries such as “how much calcium is in cheddar cheese”—look for the tag that says “Sources include: USDA”. If you have to dig deeper, look up the calcium content foods at USDA FoodData Central.
Estimate how much calcium you usually get from your diet. If you are short of the amount recommended for your age and sex, choose some of the good calcium sources suggested above to increase your intake on a consistent basis. Dairy products are ideal, because they come along with other nutrients, like protein, that are just as important for building bones, so choose them if you can. The best and most practical sources of calcium are foods that you could imagine yourself consuming every single day, such as adding one serving of lactose-free yogurt to your daily lunchbox.
Calcium SupplementsNot everyone has the option of getting calcium from milk products. If you can’t find a way to meet your calcium needs with food, ask the doctor who is treating your low bone density if you should make up the difference with a supplement. Practice guidelines for managing osteopenia and osteoporosis favor supplementation if, and only if, needed, but individuals with certain medical conditions shouldn’t take them without close medical supervision.
In all honesty, there are some unsettled questions about whether high-dose calcium supplements may be linked to heart disease or prostate cancer. You should balance these concerns against the real and present danger: you actually have a bone density problem right now, and you don’t want it to get worse. Until more is known about the possible risks, be conservative; avoid excess intake of calcium from supplements. Don’t supplement with calcium beyond your needs unless specifically prescribed by your provider. Many people find that a calcium supplement of around 400-500mg of calcium per day, together with some calcium from food, is enough.
To maximize absorption, take calcium supplements in divided doses, and choose a product that includes vitamin D. I usually recommend calcium citrate, because that form of calcium is well tolerated, can be taken with or without food, interacts with fewer medications, and is reasonably priced. It sometimes comes in “minis” or “petites” that make it easy to take 200mg twice daily. Calcium carbonate may seem attractive because it is cheaper, but some people find it causes bloating and constipation. (For this reason, don’t overdo Tums if you have IBS, because the main ingredient in Tums is calcium carbonate.) Ask your pharmacist if the calcium supplement you are considering will interact with any of your prescribed medications and when to take it to minimize interactions.
The information in the article is for educational purposes. If you need advice on your specific needs and how to meet them, consult the provider who is managing your bone health.
Further reading:Calcium Fact Sheet for Consumers, National Institutes of Health Office of Dietary Supplements. Seen at: https://ods.od.nih.gov/factsheets/Calcium-Consumer/, Jan 16, 2025.
Morin SN, Feldman S, Funnell L, Giangregorio L, Kim S, McDonald-Blumer H, Santesso N, Ridout R, Ward W, Ashe MC, Bardai Z, Bartley J, Binkley N, Burrell S, Butt D, Cadarette SM, Cheung AM, Chilibeck P, Dunn S, Falk J, Frame H, Gittings W, Hayes K, Holmes C, Ioannidis G, Jaglal SB, Josse R, Khan AA, McIntyre V, Nash L, Negm A, Papaioannou A, Ponzano M, Rodrigues IB, Thabane L, Thomas CA, Tile L, Wark JD; Osteoporosis Canada 2023 Guideline Update Group. Clinical practice guideline for management of osteoporosis and fracture prevention in Canada: 2023 update. CMAJ. 2023 Oct 10;195(39):E1333-E1348. doi: 10.1503/cmaj.221647. PMID: 37816527; PMCID: PMC10610956, seen at https://pmc.ncbi.nlm.nih.gov/articles/PMC10610956/, Jan 16, 2025.
Protecting Bone Health Among Vegans, S Palmer, Today’s Dietitian 18 (2): 24, seen at https://www.todaysdietitian.com/newarchives/0216p24.shtml, Jan 16, 2025.
This page may contain affiliate links. We are a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
June 19, 2024
FODMAPs and Protein Powders

Protein powder for your low FODMAP smoothie? Learn how to choose one.
Most people can easily meet their protein needs with food alone on a low-FODMAP diet, but sometimes a protein powder is called for. People who might be interested in using protein powers include athletes in training, people recovering from an illness or surgery, people who need soft or small-particle-size foods, small eaters, vegetarians, and anyone who enjoys smoothies. Smoothies and protein shakes are popular and delicious, but they can quickly become FODMAP bombs with the wrong protein powder in them.
Protein supplements are not right for some people, so please seek advice from your health care provider if you have medical conditions besides your IBS. The products discussed in this post are NOT meant to be sole sources of nutrition. They are called supplements because they are meant to be used in addition to a wide variety of low FODMAP foods and beverages.
The following protein supplements appear to be suitable for a low-FODMAP diet based on the listed ingredients and the nutrition info provided by the manufactures' web sites, as of this writing. They have not been lab tested for FODMAPs unless so noted. Note that other flavors by the same companies and in the same line of products may contain FODMAPs such as fructose, chicory root extract, or inulin. In the past, I kept the focus strictly on FODMAPs, but given the growing evidence that certain industrial ingredients alter the gut microbiome, promote inflammation, or increase risk for inflammatory bowel disease I am steering patients away from products that contain industrial emulsifiers, whiteners, or artificial sweeteners. Always double check the list of ingredients before you buy, because product formulations can change over time.
drink wholesome: Egg White Protein Powders and Collagen Protein Powders. I was given some free samples of the egg white protein powders and they were delicious. Egg white powder dissolves completely, has a smooth texture and tastes good. The Vanilla with Maple Sugar Protein Powder, my favorite, has real vanilla bean flavor, and is sweetened with—yes—maple sugar. Yum. Egg white protein powders are the closest you can get to a “whole food”. Certified low FODMAP by Monash University.
Jay Robb Egg White Protein: unflavored.
Now Egg White Protein: unflavored.
Nutricost Whey Protein Isolate Powder, plain or grassfed, plain. Whey protein isolates are lactose-free, because the processing removes the protein from the rest of the milk, leaving the lactose behind. There are many brands available. I am listing this one because it has a lower price point and few additives compared to some other brands.
Nutribiotic Organic Rice Protein Powder: vanilla, plain, chocolate, mixed berry. Rice protein is an “isolate”. And they can be gritty, but it is a vegan option that some individuals may prefer.
Naked Nutrition Pea Protein Isolate, plain. As with whey protein isolate and rice protein isolate, this type of protein is more highly processed that egg white protein. It is another good vegan option.
Stellar Labs Vegan Protein Powder, chocolate, vanilla. This product had protein from peas, brown rice, and quinoa. It does have a very small amount of some fruit powders in it, and a few more additives than some of the other products I’ve suggested. Certified low FODMAP by FODMAP Friendly.
There are hundreds of protein powders on the market, and they can include any and all types of FODMAPs. I can't review them all, but here are some questions to ask yourself as you try to evaluate them
What is the source of the protein?Egg whites are OK
Rice protein is OK
Whey protein isolate is OK
Whey protein concentrate is only OK if a lactose free claim is also made. 98% or better is probably fine for all but the most lactose-intolerant people.
Soy protein probably has FODMAPs
Soy protein isolate is an unknown. If truly an "isolate", then it would have been separated from the fiber in the soy, so might be OK.
Hemp protein made from powdered hemp seed is an unknown with respect to FODMAP status, though 2 tablespoons of the seeds themselves are low FODMAP.
Pea protein is low FODMAP.
What is the source of the sweetener?The best option is a plain, unflavored protein powder, to which you can add a small amount of sugar or real maple syrup. We’d all be better off if we cultivated an appreciated for less sweet flavors. If you must buy a sweetened product, stevia and monk fruit are probably OK.
Please check out my supplement shopping page to see pictures of the products I’ve recommended. With so many protein powders on the market, it makes shopping much easier to have a visual aid.
Originally published May 29, 2024. Revised and republished on June 19, 2024.
This page may contain affiliate links. We are a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
Smoothies: Easy Meals or FODMAP Bombs?
A. Smoothies have never been more popular! And why not? They taste great, they can be assembled quickly, and they offer a convenient way to have a meal while on the job or on the go.
Most of my patients have IBS, so I typically think about how smoothies fit into a low-FODMAP diet. But some have other conditions that require them to eat less roughage, or to consume a soft or small particle size diet. For these folks, smoothies are a great way to enjoy the flavors of fresh fruits and vegetables with risking trouble.
As healthy as smoothies can be, however, they have some belly-ache potential.
I recently saw a young man with a long history of IBS. His symptoms had become more severe starting about 6 months earlier. I asked him if his diet had changed around that time, and he told me a familiar FODMAP story. He had been trying to improve his diet, to eat more fruits and vegetables, and to eat more home-prepared meals. (Awesome!) His new regimen included a large smoothie every day for breakfast. (Uh-oh.) It included almost 3 cups of fruit (bananas, mixed berries, and frozen mangos), pureed with orange juice, yogurt, greens, and a sweetened protein powder. (Umm—that smoothie might explain a few things.)
Those of you who are already familiar with FODMAPs might see the problems he encountered with ingredient choices and portion sizes. If you are new to low-FODMAP eating, let’s break down smoothie logic, one element at a time:
Smoothie ComponentsLiquid: Smoothies need a liquid base. Popular low-FODMAP options include lactose-free yogurt, 99% lactose-free kefir, protein-fortified/lactose free cow’s milk, or almond milk. Skip the fruit juice—save your FODMAPs for fruit itself. Use enough liquid to help your blender do a good job grinding and pureeing the other ingredients (about 1 cup). If you don’t have IBS or are definitely not lactose intolerant, you can use regular milk products.
Ice cubes: Ice cubes are optional. Use 1/2 cup of ice cubes in your smoothie if you like an extra-cold, slushy consistency.

Use 1/2-1 cup fruit in your smoothie.
Fruit: Choose low-FODMAP servings of fresh or frozen fruit, usually about 1/2 to 1 cup (yes, really). Some popular smoothie fruits include blueberries, strawberries, and bananas, and kiwi. Frozen fruit and veggie blends are available, but avoid those which contain apples, mango, blackberries, or watermelon. If you don’t have IBS, use any fruit you like.
Vegetables: The addition of vegetables turns your drink into a “green smoothie.” While this is a great way to increase your intake of vegetables (and increase the volume of your smoothies), green smoothies can take a little getting used to. Baby spinach leaves are a “gateway” vegetable for smoothies. Start with a handful and increase as desired. Other vegetables that can be used in smoothies include carrots, cucumbers, baby kale, kale, collards, chard, arugula, and beet greens. I don’t recommend celery or celery juice as a smoothie ingredient because it is relatively high in FODMAPs.

This lovely chard would make a nice addition to a green smoothie!
Protein: For a complete meal, you may want some protein in your smoothie, in addition to the protein from the dairy ingredients you may have used as the liquid. Consider adding a scoop of lactose-free cottage cheese or a few ounces of firm tofu. Protein powders are also popular in smoothies. My favorites are made from plain or minimally processed egg whites or lactose-free whey protein, because they are low in FODMAPs and they have a great taste and texture. More about low-FODMAP protein powders.
Customize your smoothieFor a complete meal (and some soluble fiber), add 2 tablespoons of rolled oats.
For weight gain, add 2 tablespoons of peanut butter or almond butter, or up to 1 tablespoon of extra-virgin olive oil.
For more fiber, add a spoonful of chia seeds, ground flax seeds, or psyllium husk.
For anti-inflammatory effects, fresh ginger and turmeric are healthful and flavorful additions.
For a hint of sweetness, add a teaspoon of pure maple syrup or honey.
For probiotics, use a fermented milk product like kefir or yogurt as part of the liquid in your smoothie.
Double the recipes, divide in two, and save the second serving of another meal or snack later the same day.
DO you need a high-speed blender?It depends. Most people will be able to make delicious fruit smoothies with any countertop blender. But if you’ll have ongoing need for a soft, low roughage or small particle size diet, for example if you have gastroparesis or are at risk for bowel obstructions, you could think of a high-speed blender as a medical necessity. Consider a Vitamix or a Ninja. High-speed blenders are also nice to have for making vegetable smoothies because they can completely pulverize the stringy bits and seeds into a smooth liquid.
Get organized
Organize your smoothie supplies at the beginning of the week and keep them together in the refrigerator.
Preparation is the key to quickly assembling smoothies. Have all of your ingredients on hand at the beginning of the week. Group them together in an organizer bin or shoebox in your refrigerator. When it’s show time, just pull the box out and you’ll have your smoothie put together in no time. Same goes for the frozen ingredients. Prepare them ahead of time and keep them together in the freezer. For example, peel and mince fresh ginger or turmeric immediately after purchase, and freeze 1-smoothie portions in a foil twist. If you like using frozen bananas, peel, quarter and freeze a multi-day supply of them as soon as they are at the ripeness you prefer.
Build-Me-Up Breakfast SmoothieINGREDIENTS: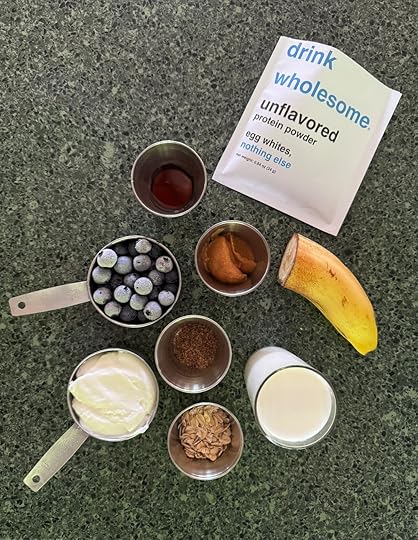
Disclosure: I was provided with a free sample of drink wholesome protein powder by the manufacturer. (It was delicious!)
2 tablespoons rolled oats
½ cup yogurt (regular or lactose-free)
½ cup milk (regular or lactose-free)
1 tsp ground flax seeds
½ cup frozen blueberries
½ banana
2 tablespoons peanut butter
1 serving protein powder
1 teaspoon pure maple syrup

The Build-Me-Up Smoothie is a small well-balanced meal.
In a blender, grind the oats into a powder. Add the yogurt, milk, flax seeds, blueberries, banana, peanut butter, protein powder and maple syrup.
Blend on high speed until smooth. If the blender blades won’t engage add some extra milk.
Serve immediately, or store in the refrigerator or a thermos for later in the day.
For a printable PDF version of this recipe, click here.
Originally published August 8, 2017. Revised and re-published June 19, 2024.
This page may contain affiliate links. We are a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
Low-FODMAP Certification Programs

Label reading is difficult enough in your own kitchen, and more so in the aisles of a busy grocery store.
It would be lovely to be able to make everything we eat from absolute scratch, but few of us have the time or the inclination to do so. Even if you tend to think “processing” is a dirty word, be honest—when was the last time you made your own cheese, ground your own flour, or cracked the shells off your own nuts? So, we all need to learn how to read food labels to determine which prepared foods are low in FODMAPs.
One approach to this task is to carefully read the ingredients statement on the label and avoid products that have known high-FODMAP ingredients in them. This usually works, but has shortcomings. It is time consuming. We don’t know the FODMAP status of some ingredients. Hidden FODMAPs can be present. For example, the word “flavorings” in a soup or broth can be hiding some onion or garlic juice. The amount of the high-FODMAP ingredient might be so small that rejecting the food because of its presence might be overkill.
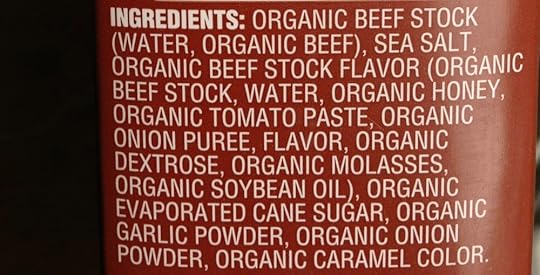
Carefully read the list of ingredients and compare each one to your list of high- and low-FODMAP foods to see if it is suitable for your low-FODMAP diet. This task can leave you wishing for a product clearly marked with a low-FODMAP certification! (Tip: Organic is nice if you can afford it, but not relevant to decision-making for a low-FODMAP diet. This particular beef stock is probably high in FODMAPs.)
Third-party low-FODMAP certification programs have come to your rescue! Several certification programs are now widely in use. Certifications can relieve you of the detailed label reading and guesswork. I can’t speak for the situation in other countries, but here’s what you need to know if you live in the United States. Low-FODMAP certification programs are:
Voluntary. If the manufacturer of a food product wants a certification, they pay an independent organization to have it laboratory tested, data compared to set criteria, and certified. They may pay additional fees to display the related seal on their food products or to be included in the related iOS or Android app.
Not federally defined by the US Government. Unlike claims like “organic” or “gluten-free,” the federal government has not defined what “low-FODMAP” means or which foods can claim to be low-FODMAP. Each certification program has its own set of criteria for “low-FODMAP.”
Only as good as the organization that backs them up. Consumers need to ask themselves whether the certifying institution, business or laboratory is truly independent, trustworthy, and has a transparent and science-based process.
Two low-FODMAP certification programs that I trust are administered by Monash University and FODMAP Friendly. Even though these programs are based in Australia, they are certifying products made and sold in the United States, among other places. Rather than risk giving incorrect or dated information about these programs, I’m going to send you directly to their respective web sites for more information, and to see what the seals look like:
Monash University Low FODMAP Certification Program
One of my patients recently admitted to me, “I work full time, and have three kids—one with special needs. I just didn’t have time for label reading. I’m sorry, but I couldn’t fully follow the low-FODMAP diet you asked me to try.” For people like her, low-FODMAP certified groceries can’t materialize on the shelves of the local grocery store soon enough. Until then, I reminded her to check my shopping pages for groceries, baking supplies, and supplements. These pages do include some low-FODMAP certified foods; the rest I consider suitable for low-FODMAP diets based on my reading of the list of ingredients.
Originally published February 5, 2017. Revised and re-published June 19, 2024.
This page may contain affiliate links. We are a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
February 17, 2024
Is date sugar low FODMAP?
A. The short answer: as of this writing, we can only guess about the FODMAP status of date sugar. It probably has a small low FODMAP serving size, less than 2 tablespoons.

Is date sugar low FODMAP?
Date sugar is made from ripe, pitted dates that are dried to a very low moisture content and ground into a powder. Dates are the fruits from certain types of palm trees. But date sugar is not the same as palm sugar, which is made from the sap of palm trees. The Monash University FODMAP lab has analyzed “dried dates” in general, and one specific variety (Medjool), but not date sugar, the packaged sweetener.
We see in the Monash University Low FODMAP app that somewhere between 1 and 5 dates, or .71 oz to 1.06 oz of dates are low FODMAP. It’s difficult to guess how this information equates to date sugar.
Dates vary in nutritional compositionThere are hundreds of varieties of dates grown around the world. In Saudi Arabia alone, there are over 300 varieties of dates grown, and they vary significantly in sugar and moisture content. Other countries and regions have their own unique varieties of dates. The variety of date used isn’t usually specified by the manufacturers of date sugar, but the moist varieties meant for snacking on are not likely to be among them. Therefore, It isn’t likely that date sugar has the same FODMAP content as the dates that were analyzed for FODMAPs at Monash.
Serving size estimatesWe don’t know how much moisture is lost, or how much the ground dates “fluff up” in the making of date sugar. So if we said, for the sake of argument, that the type of sugar was similar to the dates in the app, we would have to figure many teaspoons or tablespoons of date sugar would equal the amount of FODMAPs in 1 pitted date. My calculations suggest that 2 tablespoons of date sugar has about the same amount of total sugar as one Medjool date.
Effects of ripening and dryingAdding more uncertainty, the final stages of ripening and drying of foods can alter their FODMAP content in unpredictable ways (check out the difference between grapes and raisins, or rice and puffed rice). As dates ripen, much of the sucrose content is “inverted”, or broken down to glucose plus fructose. Does that continue or change during the further drying of dates for grinding? It’s anyone’s guess. To be on the safe side, my guess will be conservative. Pending actual lab analysis of date sugar, less than 2 tablespoons might be low in FODMAPs. Larger servings might be a significant source of sorbitol and fructans.
ConclusionLike many foods, dried dates can actually be low, medium, or high in FODMAPs depending on the serving size. Dates meant for eating have been lab tested, but date sugar has not. If you’d like to bake with date sugar on your low FODMAP diet, my advice is to make sure there’s less than 2 tablespoons in your portion of the recipe.
Further reading:AlShwyeh H, Almahasheer H. Glucose content of 35 Saudi Arabian date fruits (phoenix dactylifera L.), Journal of the Saudi Society of Agricultural Sciences 21 (2022) 420-424. Seen at: https://www.sciencedirect.com/science...
January 28, 2024
Why Not Stay Low FODMAP Indefinitely?
The short answer is that a Low FODMAP diet may be too limited in some cases. More variety, usually results in a more nutritious diet and promotes a better food quality of life.
In many ways it is so much simpler to just follow the rules and stay low-FODMAP than it is to go through the uncertainly of the reintroduction process. But simple isn’t always easy, is it? In fact, most of my practice these days, almost 15 years into the FODMAP era, consists of helping people take those next important steps toward a varied diet. Why bother?
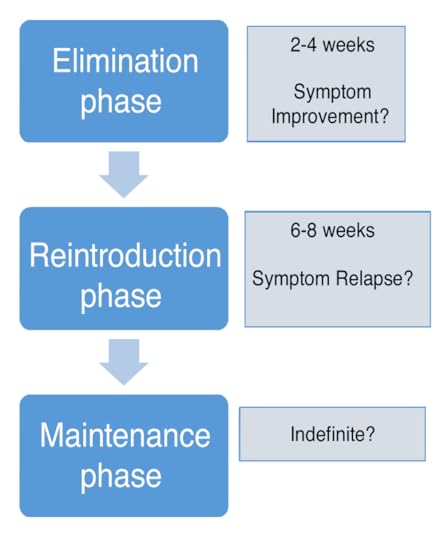
Ideally, the FODMAP elimination diet is a short dietary experiment. Eswaran SL Curr Opin Pharmacol, 2017
As you have read, low-FODMAP diet is meant to be a short dietary experiement, to get IBS symptoms under control. If it doesn’t work for you, don’t continue it. If it does improve your abdominal and bowel symptoms, it should be followed by a reintroduction process. That is the only way to figure out which FODMAPs are (and are not) symptom triggers for YOU. They are not the same for everyone. This paves the way for you to enjoy a more varied diet.
A Varied Diet is more nutritiousFortunately, there are good low-FODMAP sources of all nutrients. So if you are willing and able to eat a wide variety of low-FODMAP foods you might not have to worry too much about this one. But, if you add other dietary restrictions, you can find yourself eating a repetitive, short list of foods that comes up short in some areas. For example, it can be difficult for vegans to get enough protein on low-FODMAP diets, if they are used to eating a lot more beans, nuts and seeds. Other people might be at risk for poor intake of certain nutrients even on their usual diets, in ways that have less to do specifically with FODMAPs. For example, people on dairy-free diet rarely get the recommended amounts of calcium from food. People who don’t care for green leafy vegetables or nuts probably aren’t consuming enough magnesium, and so on.
Some FODMAPs are important prebioticsFructans and GOS are two of the six FODMAPs that are limited on low-FODMAP diets. They are also well-known prebiotics. Prebiotics are selectively fermented by the “good” bacteria in you gut, to produce beneficial substances like short chain fatty acids. When you are on a low-FODMAP diet you cut back on these a great deal.. Hopefully you are still eating low-FODMAP servings of foods that contain some fructans and GOS, along with good low-FODMAP sources of prebiotics. Choose low-FODMAP servings of whole grains, fruits, vegetables, nuts, seeds, and legumes. After the reintroduction process, you should eat larger servings of these foods if you can tolerate them, to increase your intake of prebiotics.
Food Quality of Life
Sharing is an important part of “food quality of life”. Photo credit: C. Catsos
Most people find that their food quality of life is better when they are eating a more varied diet. What does this mean? It means being able to share in communal food life and (mostly) eating what is served when dining with friends and family. It means not having to say “no” to everything just because you are following the rules, and not having to bring your own meals to gatherings. It means enjoying occasional restaurant meals with more confidence. It means generally just having a better relationship with food and being less afraid of food and eating. My patients who have figured out what
Be SureYour question indicated you “feel like” low FODMAP diet keeps your IBS under control and “may be helping”. You need to be more certain than that to justify the potential drawbacks of a long term low FODMAP diet. Self-knowledge is your ticket forward. Gain it by reintroducing FODMAPs in a structured way, monitoring symptoms, then adjusting your diet as tolerated.
This page may contain affiliate links. We are a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
January 12, 2024
What Spices Can I Use on a Low FODMAP Diet
A. The short answer if that most herbs, spices, and flavorings can be used on a low FODMAP diet. Don’t worry about spices, except those containing onion or garlic.
Determining the FODMAP StatusInformation about the FODMAP content of herbs, spices, and flavorings comes from the FODMAP lab at Monash University. Because they know it’s a tall order to make food without onions or garlic, the Monash team has invested a lot of effort into testing herbs and spices from around the world. Several samples of each individual item are collected, pooled together, and freeze-dried, then tested with specialized laboratory equipment. The results are translated into the Monash University Low FODMAP app where low FODMAP servings are labeled with a green light. You will find that some herbs or spices can be low, medium, or high FODMAP depending on the serving size.
The Alliums
Bulbs of onions, garlic, and shallots are high in FODMAPs.
Onions, garlic, and shallots, members of the allium family, are especially significant sources of FODMAPs. There are no low-FODMAP serving sizes for most of them. It doesn’t matter how little you use! Even onion and garlic powder or flakes should be eliminated on a low-FODMAP diet. Leek bulbs are the exception. They do have a low-FODMAP portion size of 1 tablespoon. Beware of spice blends, which often include onion and garlic pieces or powders.
Ordinary cooking and bakingIn the amounts used in the United States for everyday cooking and baking, that vast majority of herbs, spice, and flavorings are low-FODMAP or have low-FODMAP serving sizes. A few herbs or spices are used in larger amounts. Even then, your individual portion of the recipe is unlikely to contain more than a teaspoon of cinnamon, cumin, or chile powder, the typical low-FODMAP serving size for such things. If you cook with or eat entire chile peppers, check the app for details on low-FODMAP serving sizes.
Other flavoringsFresh lemon juice, fresh lime juice, and most vinegars are also low-FODMAP when used in ordinary amounts (balsamic vinegar has a limited low FODMAP portion). They can add so much lively flavor to your recipes! The green parts of scallions, leeks and garlic (scapes) are low in FODMAPs, too. Prepared condiment should be considred on a case-by-case basis. Most soy sauces, tamari, prepared mustards, and certain vinegar-chile hot sauces don’t have high FODMAP ingredients. But many other condiments and salad dressings do contain onion, garlic, or high-fructose corn syrup so read labels carefully. Choose brands that don’t have high FODMAP ingredients or those that have been lab-tested to check their FODMAP status. Several brands of low-FODMAP specialty foods are available, with seasoning blends, salsas, and sauces that add lots of flavor to you low-FODMAP diet.
Medicinal useIf you are taking large amounts of an herb or spice for some medicinal purpose, you will have to pay more attention to the limits on the low FODMAP serving sizes. Please refer to the Monash University FODMAP Diet app for specific limits.
Shop for low-FODMAP groceries here.
This page may contain affiliate links. We are a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
December 20, 2022
Can IBS Lead to Other Conditions?
A. The sort answer: irritable bowel syndrome (IBS) does not cause other conditions.
As thinking people, we feel a strong need to connect the dots, to understand the reasons things happen, to ask why? Was IBS the reason we developed another condition? Would treating our IBS differently have prevented the other disease in the first place? Will IBS will lead to health problems in the future?
The S in IBS stands for syndrome, which is essentially a collection of symptoms. IBS is defined by symptoms of recurring abdominal pain, diarrhea, constipation, or alternating bowel habits, at least one day a week over the last 3 months, with symptom onset at least six months before the diagnosis. Symptoms are things the patient experiences. They may (or may not) reveal the existence of an underlying disease or disorder. Symptoms don't cause diseases. It is the other way around. Diseases cause symptoms.
CauseThe cause of a disease is the reason it develops. IBS is not the reason that diseases occur. Fortunately, there isn't any reason to think that having IBS means your gastrointestinal problems will get worse over time or turn into another condition. To answer some specific questions I have received from my readers, a diagnosis of IBS is not believed to cause diverticulitis, megacolon, cancer, Crohn's disease, ulcerative colitis, celiac disease, thyroid problems, autoimmune disorders, or fibromyalgia.
There is some gray area when it comes to anxiety and depression. You may certainly be anxious or stressed about your IBS, or feel depressed or sad about how IBS is affecting you. This type of anxiety or depression may be described as situational. Situational anxiety and depression are different from generalized anxiety disorder and clinical depression. The latter are more chronic; they would exist even in the absence of difficulty adjusting to the impact IBS has on you..
Symptoms themselves can occasionally cause complications. For example, constipation could be at least a partial cause of hemorrhoids, anal fissures, or rectal prolapse. Severe diarrhea can contribute to dehydration or electrolyte imbalance.
AssociationAssociation means that some health conditions are more likely to occur in the same population of people. For example, as a group, people with IBS are more likely to be diagnosed with gastroesophageal reflux disease (GERD) than people who don't have IBS. But it cannot be said that IBS is the reason for the GERD. People with IBS are more likely than people without IBS to be diagnosed with clinical depression or chronic pain conditions. They more frequently have additional disorders affecting the stomach, esophagus, or anorectal parts of the gastrointestinal tract.
Diverticulitis is strongly associated with IBS. There is a possibility that the diverticulitis causes IBS or IBS-like symptoms, but the reverse is not likely.
IBS and eating disorders are unquestionably associated. About half of patients with eating disorders also have IBS. And some people with IBS may develop disordered eating habits as a way of avoiding symptoms.
Delayed Diagnosis or MisdiagnosisThe difficulty that you and you healthcare providers may face is that many diseases share the symptoms of IBS. Abdominal pain, bloating, diarrhea, and constipation are far from unique to IBS. So there are a certain number of people who are diagnosed with IBS who turn out to have a different diagnosis that explains their symptoms. For example, C. difficile colitis, diverticulitis, celiac disease, inflammatory bowel disease, exocrine pancreatic insufficiency, cancer, or eating disorders could seem like IBS at first. That is why it's important to be evaluated by a medical professional rather than diagnosing yourself with IBS. Make sure your provider knows about any "alarm features" you have that would call for more tests or procedures to rule out other conditions. Alarm symptoms to report include: bloody, oily, very frequent or watery stools; fever; unintentional weight loss; abnormal laboratory results; or bloating or abdominal pain that never goes away. And share any concerns you may have about your eating thoughts or behaviors.
References:Aziz, I et. al. The prevalence and impact of overlapping Rome IV-diagnosed functional gastrointestinal disorders on somatization, quality of life, and healthcare utilization: A cross-sectional general population study in three countries. Am J Gastroenterol 2018.;113(1), 86–96.
Cohen, E et. al. Increased Risk for Irritable Bowel Syndrome after Acute Diverticulitis. Clin Gastroenterol Hepatol 2013; 11(12): 1614-1619.
Riehl, M and Scarlata, K. Understanding Disordered Eating Risks in Patients with Gastrointestinal Conditions. J Acad Nutr Diet 2022; 122(3), 491-499.
November 14, 2022
Should I Start my Low-FODMAP Diet Before or After the Holidays?
A. It's your call, of course, but many people find a way to follow low-FODMAP diets during the holidays so they can feel their best on special occasions and vacations. A few limited exceptions to the diet will not ruin your low-FODMAP diet. Just get right back on track at the next meal or snack and carry on.
You have choicesHas your doctor or dietitian recommended that you try a low-FODMAP diet for your irritable bowel syndrome (IBS)? If so, you might be wondering when to begin. Special occasions and vacations occur year-round, don't they? There is almost always some upcoming event or activity that will require some adjustments to your low-FODMAP diet, and the upcoming holiday season is no exception!
Ask yourself how important it is for you to keep your symptoms to a minimum during the holidays. The prospect of feeling well during the holidays for a change can be very motivating! If that sounds like an amazing possibility, go ahead and start your low-FODMAP diet now. This choice does mean that you'll have to enjoy foods a little differently this year, but luckily, many holiday favorites are naturally low-FODMAP or can be easily adapted.
On the other hand, you might choose to set a starting date after the holidays if your IBS symptoms are mild, or if you'd rather suffer the consequences than eat differently from your usually holiday fare. In that case, you can still use the time available between now and then to learn about FODMAPs, and to get your meals and groceries organized.
Exceptions TO Low-FODMAP Diet for special occasionsIf you're an over-achiever or a perfectionist, hear me now: a low-FODMAP diet does not have to be perfect to be a good learning experience or to improve your IBS symptoms over the long run. The goal of the Elimination Phase of the diet is to greatly reduce your intake of FODMAPs to see if it helps, not to be a master rule-follower. Yes, you will learn more the closer you stick to the low-FODMAP diet overall during the Elimination Phase. But some limited exceptions will not ruin the whole project. Symptoms might be occur in the immediate aftermath of a higher FODMAP meal though, depending on how big the exceptions are.
It's OK to eat mostly low-FODMAP at a holiday meal while allowing yourself an exception for something really special. You might get away with this rather well if you've left plenty of room in your FODMAP "bucket" by choosing low-FODMAP foods and serving sizes for the rest of the meal.
It's even OK to make the whole meal an exception, though this approach is more likely to lead to a significant bout of IBS symptoms in those who are intolerant to FODMAPs. It's your call. Just keep portions on the small side, get back on track ASAP, and consider it a learning experience if you don't feel well later.
Holiday baked goodsHoliday baking is a beloved tradition in many families, and most people following a low-FODMAP diet would be loathe to let the season pass without enjoying a few cookies or other family favorites. Unfortunately, wheat-based flour (whether it be white, all-purpose, or whole wheat) is a significant source of fructans, one of the FODMAPs. You have a choice of two strategies for working around this.

Enjoy these delightful Low-FODMAP Sugar Cookies!
The first option is to make low-FODMAP versions of the recipes, using gluten-free flours instead of regular flour. Gluten is not a FODMAP, so avoiding gluten isn't the point of using gluten-free flour in this case. The alternative flours happen to be lower in FODMAPs, so they are more suitable for a low FODMAP diet. Pro-tip: for best results, use recipes that were developed by an expert to match the baking characteristics of a particular gluten-free flour or blend. You will probably not be as happy with merely substituting a gluten-free flour or blend for the regular flour in your favorite recipe. Maybe you’ll enjoy my own Low-FODMAP Sugar Cookies! See our articles on gluten-free flours for secrets to success!
The second option is to limit yourself to low-FODMAP serving sizes of a plain cookies or cake (without fruit or nuts) at any one meal or snack, which is probably about 1/2 ounce, or a 2-inch diameter cookie. This suggestion is based on a bit of guesswork, since very few cookies (biscuits) have been analyzed at the Monash FODMAP lab. Put some cookies in the freezer and have a few during the Reintroduction Phase when you introduce fructans!
Whatever you decide to do, I wish you well, and Happy Holidays!
Resource:Shop Low FODMAP: Baking Supplies



