Covid-19 and me
I’m currently in the process of recovering from Covid-19, and beyond grateful to be able to write the first part of this sentence. I know others who have been through it too, and for each of us it seemed a bit different. While the grim coronavirus experience is still all-too-fresh in my mind, here are some of the things that helped me get through. If you’re unlucky enough to get Covid-19, you may find some parts of my experience useful, or you may not. I’m well aware that nothing is certain with Covid-19 and that what I write here will be contradicted by someone else’s experience. That is how this virus seems to work.
Firstly, I should say I’m a previously fit and healthy 60-year-old white man living in north London with his wife and two young-adult daughters. I cycle, I run, I’m a stranger to hospitals (apart from during my lightning appendix adventure in Switzerland a couple of years ago, but that’s another story). I work at a university in central London, and I draw and write.
None of this is advice. This is just what helped me. What worked for me may well not be right for you. And advice will, no doubt, develop as more is understood about Covid-19.
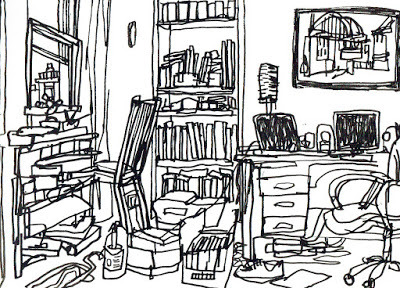 The view from my isolation bed, drawn on day 62
The view from my isolation bed, drawn on day 62
Day 1: I’m not even entirely sure when it started, although 26 March 2020 is marked in my diary. I was working from home from mid March and not long after I didn’t feel quite right. I was tired and achey, but it coincided with the inevitable stress of getting geared up for working from home, and the emotional element of the world changing before our eyes in the most unreal, dreamlike way. We are lucky to have a foldout bed in the workspace at the top of the house where I could isolate myself.
My symptoms at the start? Aches, tiredness, a tightness of the chest, an occasional fluttering (odd to call it that, but that’s how it felt) in the top of my chest, occasional sharp spasms of pain in my limbs and abdomen that disappeared as soon as they arrived, and occasional raised heart rate. I never had either the dry cough or the fever (I woke one night in a sweat, but I still think that was a different duvet issue rather than a fever). This confused us. Official UK information said at that time that without those two symptoms it was unlikely you had Covid-19. Later, the loss of smell and taste was added to the list: I never had that as a symptom either. Did I just have regular flu? At some point, by which point I had already isolated myself, it became obvious it was Covid-19 that I had. The increasing breathing difficulties and fatigue seemed the most obvious signs.
Days 2-8: In bed, keeping as still as possible, tackling increasing waves of breathlessness, sleeping, and keeping anxiety at bay. The breathlessness could come while I was sitting or lying quietly. The worst part was not knowing if this was part of process of deterioration. Anxiety and breathing difficulties is not an enjoyable combination. Distraction techniques – TV series of a gentle humorous variety (The Detectorists, This Country), reruns of old cricket Tests on Radio 5 Live, football repeats of old international matches, and Mindful Mixes on BBC Sounds helped me through. Trips down the stairs to the first-floor bathroom were very slow, and fraught with worries about contamination. Door handles, light switches, flush handles, towels, toothpaste: we cleaned and segregated as we could. The way in which I am most lucky in this whole story is with the people I share my life with, who brought love and attention, food and drink to me, daily, hourly, and who thought straight when I couldn’t.
Day 9: I thought I was improving a little. I got up on day 9, made porridge, put out the recycling, all very gently. Whether this resulted in or merely coincided with my first relapse I’m not sure, but I was soon back in bed and feeling worse than during the first eight days.
Days 10-67*: This was the start of my worst time, physically and mentally. Cases and deaths in the UK were rising exponentially at this point, and the prime minister was taken into intensive care. There were the sounds of sirens outside, and the girls were leaving food at my door. My symptoms were still spells of shortness of breath, tight chestedness, fatigue. We rang the NHS 111 line during this time, and also our GP, who rang me daily for a while during my worst spell. A process of improvement and relapse in a slowly improving way has continued since about day 22. Days pass without breathlessness, and then return. The fatigue is a constant over this time. (* I'm on day 67 as I write.)
Here are some things that helped me through this time of Covid-19 and recovery.
Drinking water, lots: I heard people were recommended three litres a day, but I could only manage two litres. Sipping slowly eased, momentarily, the feeling of tightness in the throat. The mouth dries out quickly if you’re breathing through your mouth as you lie and rest.
Breathing exercises, clearing lungs, mental health: I found some information through links sent to me via different NHS sources. The Lancashire Teaching Hospitals NHS Foundation Trust have great info on dealing with Covid-19 recovery. And this one on breathing exercises from doctors at Queen's Hospital, London, was sent via a family member early on in lockdown.
Distractions: As I’ve mentioned, TV and radio of the most gentle and escapist kind helped from time to time. For a while I escaped via the Antiques Road Show and the quiz show Pointless: this has now, mercifully, passed, but they helped me through. Nothing is off limits if it helps you get through.
Friends and relations: It was lonely being at the top of the house, even though I had my family at hand. Respect to those who are going through this alone! Honestly, nobody knows what they are going through. Strength to you if you are reading this now! I was messaging friends and family, replying to their requests for updates, and we had a London family WhatsApp group to share information about each other. I have a good friend going through a very similar experience to mine at exactly the same time, which is useful, if unfortunate. We share things as we come across them.
Support group: I came across the Body Politic Covid-19 support group on day 36 via a reference in a Guardian article. It is a Slack group - you request to join and are sent a link to access it, and to introduce yourself, using the relevant channels. It was a such relief to find this group of people having similar experiences to me. Through this you can find links to useful research, articles, polls, links and current thinking. I mostly interacted in the UK channel, where I found people related to things in a way similar to mine. Many of the group’s members are in the US, particularly in New York, where the medical jargon and systems are very different to those in the UK. There are elements of the group, of course, that you may want to avoid. It’s a great place to ask questions and get useful advice, but there’s also the danger of finding new things to worry about. There are channels for #victories and #positivity, which can lift the soul and offer optimism. This forum was the place that helped me not feel alone. Hail its founders.
Diet: Skip inflammatory foods. It’s easy to search for what this means.
Vitamin D and zinc: These may not help fight off Covid-19, but I took them most days anyway. A good balanced diet seems most effective in terms of boosting immunity.
https://covid.joinzoe.com/post/vitamin-supplements-covid
Manuka honey: Does it do anything to help? Probably not, but a spoonful or two a day tasted great.
Inhalations: A bowl of boiling hot water, with a few drops of thyme essence, a towel over the head, and the Max Richter Mindful Mix on BBC Sounds. Deep breaths in the dark heat. This, more than anything, was my escape.
Sitting out: A chair in the sun on the doorstep on better days with the Guardian crossword. Friends and neighbours would stop to chat over the gate from a safe distance. This was great.
Articles: You’ll find links to up-to-date ones on the Body Politic support group’s #resources channel. The ones that were a particular support for me were:
We need to talk about what coronavirus recoveries look like, New York Times, 13 April 2020
https://www.nytimes.com/2020/04/13/opinion/coronavirus-recovery.html
Lingering and painful: the long and unclear recovery to coronavirus recovery, The Guardian, 1 May 2020
https://www.theguardian.com/world/2020/may/01/lingering-and-painful-long-and-unclear-road-to-coronavirus-recovery-long-lasting-symptoms
Paul Garner: for seven weeks I have been through a roller coaster of ill health…, BMJ blog, 5 May 2020
https://blogs.bmj.com/bmj/2020/05/05/paul-garner-people-who-have-a-more-protracted-illness-need-help-to-understand-and-cope-with-the-constantly-shifting-bizarre-symptoms/
Hospitalisation: I never went to hospital, mainly because I wasn’t ill enough. We rang 111 on day 18 when things were bad, but by speaking to me they could tell my breathing difficulties weren’t enough to admit me. Perhaps this was good news, but I really wanted some medical expertise at this point. They took our details so a doctor could ring back to speak to me: the return call never came. My second 111 call on day 51 was similarly unhelpful (I’ll spare you the tale of the wasted hours on that call). My local GP was more accessible and supportive…
My local GP: Our local surgery in Stoke Newington was great, and they readily admitted they were still learning how to handle Covid-19 at this early stage. They rang me daily for a while during my worst spell. I think it’s good to be in contact with your GP, and see what they can do for you in your situation. On day 30 I was checked for oxygen levels and heart rate in the carpark behind the surgery (I shuffled slowly up the pavement with N for this rather bizarre but appreciated back-door appointment), and on day 54 I finally had a face-to-face meeting with my GP. They examined me thoroughly for secondary infections and sent links to two useful resources with details of recovery support from our local hospital and Covid 19-related research:
Post Covid-19 Patient Information Pack from Homerton University Hospital NHS Foundation Trust:
https://mcusercontent.com/30db5cb77411d59f467a2fecf/files/5fe19213-796d-4e9d-a04e-af9ab02c2acd/FYI_2_Post_COVID_19_information_pack.pdf
Oxford Covid -19 Evidence Service: regularly updated coronavirus evidence reviews, data analysis and writing:
http://www.cebm.net/oxford-covid-19-evidence-service/
Medication: It was paracetamol primarily. I became aware, through the support group, of other users taking medication (omeprazole) for silent reflux, which has similar symptoms to some related to Covid-19. I discussed this with my GP and started a four-week course of them on day 39, which helped. Compared to the cornucopia of medication some people obviously have taken, mine is small fry.
Crosswords, genealogy: sitting in the sun on a sofa turned to face out the front window, keeping still and calm, these two were a good balance of gentle and stimulating.
Things I didn’t do no.1: draw. I tried, but I just couldn’t do it. It was too much, and creativity dipped. I have a few bad unfinished drawings from this time. The first thing I was able to draw was my stubble.
Things I didn’t do no.2: read. I would fall asleep rather than read. American Marriage by Tayari Jones lay half read by my bed the whole time.
Things I didn’t do no.3: exercise. Over and over on the support group I would read about fit people recovering from the virus who resumed running 5km or even 10km at the first symptom-free day, and who then reported immediate relapses. I have taken short, gentle walks but no more.
News and media: I couldn’t bring myself to listen to news reports much - it fed anxiety, and I was aware that N and the girls would pick up on anything important and let me know. As much as anything, I needed to keep positive, and updates on the exponential growth of Covid-19 cases and deaths was not good for the mind.
Social media: I generally avoided it. I didn’t want to read about the wonderful creative opportunities that lockdown presented to us all, or badly researched medical stories too easily shared. I wanted useful practical information straight from the trusted expert source, although being so early on in the pandemic’s timeline even the most reliable sources were scrabbling around trying to get to grips with what we are dealing with. (That’s still true now, two months on as I write this.)
Reporting symptoms: Very early on I started reporting my symptoms on the world’s largest study of the virus, the Covid-19 Symptom Study app. Its website is good for essential Covid-19 reading and research.
Applauding the NHS every Thursday at 8pm: I recorded the second of these when things felt at their darkest for me. It was great to hear people whoop and holler in the buildings and streets around. N and the girls were in the windows below and or the doorstep joining in, not that I could see them. It was a great moment of connection early on, pre-Cummings, at a point when we really thought we were all in it together.
If you get Covid-19, it seems most likely you’ll get it mildly and recover quickly, or perhaps not even know you have had it. We all know that age, race, sex and other health issues play their parts in how seriously we get it. I expected, naively, that I would get through Covid-19 quite quickly. It didn’t turn out like that, as I have hinted. I am lucky that I have my family to support me through it all in ways I’ll never forget, that my employers are so understanding and supportive, and that, although it has stayed with me a long time, my own Covid-19 wasn’t serious enough to deliver me to intensive care. But of course you don’t know that when you’re going through it in the darkness, just as we don't know where it will lead us from here.
Most of all, stay well.
Firstly, I should say I’m a previously fit and healthy 60-year-old white man living in north London with his wife and two young-adult daughters. I cycle, I run, I’m a stranger to hospitals (apart from during my lightning appendix adventure in Switzerland a couple of years ago, but that’s another story). I work at a university in central London, and I draw and write.
None of this is advice. This is just what helped me. What worked for me may well not be right for you. And advice will, no doubt, develop as more is understood about Covid-19.
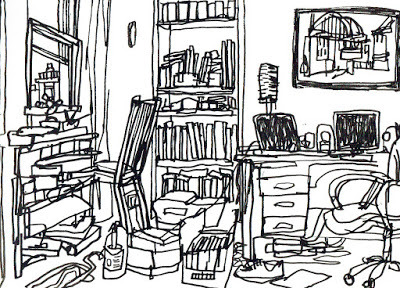 The view from my isolation bed, drawn on day 62
The view from my isolation bed, drawn on day 62
Day 1: I’m not even entirely sure when it started, although 26 March 2020 is marked in my diary. I was working from home from mid March and not long after I didn’t feel quite right. I was tired and achey, but it coincided with the inevitable stress of getting geared up for working from home, and the emotional element of the world changing before our eyes in the most unreal, dreamlike way. We are lucky to have a foldout bed in the workspace at the top of the house where I could isolate myself.
My symptoms at the start? Aches, tiredness, a tightness of the chest, an occasional fluttering (odd to call it that, but that’s how it felt) in the top of my chest, occasional sharp spasms of pain in my limbs and abdomen that disappeared as soon as they arrived, and occasional raised heart rate. I never had either the dry cough or the fever (I woke one night in a sweat, but I still think that was a different duvet issue rather than a fever). This confused us. Official UK information said at that time that without those two symptoms it was unlikely you had Covid-19. Later, the loss of smell and taste was added to the list: I never had that as a symptom either. Did I just have regular flu? At some point, by which point I had already isolated myself, it became obvious it was Covid-19 that I had. The increasing breathing difficulties and fatigue seemed the most obvious signs.
Days 2-8: In bed, keeping as still as possible, tackling increasing waves of breathlessness, sleeping, and keeping anxiety at bay. The breathlessness could come while I was sitting or lying quietly. The worst part was not knowing if this was part of process of deterioration. Anxiety and breathing difficulties is not an enjoyable combination. Distraction techniques – TV series of a gentle humorous variety (The Detectorists, This Country), reruns of old cricket Tests on Radio 5 Live, football repeats of old international matches, and Mindful Mixes on BBC Sounds helped me through. Trips down the stairs to the first-floor bathroom were very slow, and fraught with worries about contamination. Door handles, light switches, flush handles, towels, toothpaste: we cleaned and segregated as we could. The way in which I am most lucky in this whole story is with the people I share my life with, who brought love and attention, food and drink to me, daily, hourly, and who thought straight when I couldn’t.
Day 9: I thought I was improving a little. I got up on day 9, made porridge, put out the recycling, all very gently. Whether this resulted in or merely coincided with my first relapse I’m not sure, but I was soon back in bed and feeling worse than during the first eight days.
Days 10-67*: This was the start of my worst time, physically and mentally. Cases and deaths in the UK were rising exponentially at this point, and the prime minister was taken into intensive care. There were the sounds of sirens outside, and the girls were leaving food at my door. My symptoms were still spells of shortness of breath, tight chestedness, fatigue. We rang the NHS 111 line during this time, and also our GP, who rang me daily for a while during my worst spell. A process of improvement and relapse in a slowly improving way has continued since about day 22. Days pass without breathlessness, and then return. The fatigue is a constant over this time. (* I'm on day 67 as I write.)
Here are some things that helped me through this time of Covid-19 and recovery.
Drinking water, lots: I heard people were recommended three litres a day, but I could only manage two litres. Sipping slowly eased, momentarily, the feeling of tightness in the throat. The mouth dries out quickly if you’re breathing through your mouth as you lie and rest.
Breathing exercises, clearing lungs, mental health: I found some information through links sent to me via different NHS sources. The Lancashire Teaching Hospitals NHS Foundation Trust have great info on dealing with Covid-19 recovery. And this one on breathing exercises from doctors at Queen's Hospital, London, was sent via a family member early on in lockdown.
Distractions: As I’ve mentioned, TV and radio of the most gentle and escapist kind helped from time to time. For a while I escaped via the Antiques Road Show and the quiz show Pointless: this has now, mercifully, passed, but they helped me through. Nothing is off limits if it helps you get through.
Friends and relations: It was lonely being at the top of the house, even though I had my family at hand. Respect to those who are going through this alone! Honestly, nobody knows what they are going through. Strength to you if you are reading this now! I was messaging friends and family, replying to their requests for updates, and we had a London family WhatsApp group to share information about each other. I have a good friend going through a very similar experience to mine at exactly the same time, which is useful, if unfortunate. We share things as we come across them.
Support group: I came across the Body Politic Covid-19 support group on day 36 via a reference in a Guardian article. It is a Slack group - you request to join and are sent a link to access it, and to introduce yourself, using the relevant channels. It was a such relief to find this group of people having similar experiences to me. Through this you can find links to useful research, articles, polls, links and current thinking. I mostly interacted in the UK channel, where I found people related to things in a way similar to mine. Many of the group’s members are in the US, particularly in New York, where the medical jargon and systems are very different to those in the UK. There are elements of the group, of course, that you may want to avoid. It’s a great place to ask questions and get useful advice, but there’s also the danger of finding new things to worry about. There are channels for #victories and #positivity, which can lift the soul and offer optimism. This forum was the place that helped me not feel alone. Hail its founders.
Diet: Skip inflammatory foods. It’s easy to search for what this means.
Vitamin D and zinc: These may not help fight off Covid-19, but I took them most days anyway. A good balanced diet seems most effective in terms of boosting immunity.
https://covid.joinzoe.com/post/vitamin-supplements-covid
Manuka honey: Does it do anything to help? Probably not, but a spoonful or two a day tasted great.
Inhalations: A bowl of boiling hot water, with a few drops of thyme essence, a towel over the head, and the Max Richter Mindful Mix on BBC Sounds. Deep breaths in the dark heat. This, more than anything, was my escape.
Sitting out: A chair in the sun on the doorstep on better days with the Guardian crossword. Friends and neighbours would stop to chat over the gate from a safe distance. This was great.
Articles: You’ll find links to up-to-date ones on the Body Politic support group’s #resources channel. The ones that were a particular support for me were:
We need to talk about what coronavirus recoveries look like, New York Times, 13 April 2020
https://www.nytimes.com/2020/04/13/opinion/coronavirus-recovery.html
Lingering and painful: the long and unclear recovery to coronavirus recovery, The Guardian, 1 May 2020
https://www.theguardian.com/world/2020/may/01/lingering-and-painful-long-and-unclear-road-to-coronavirus-recovery-long-lasting-symptoms
Paul Garner: for seven weeks I have been through a roller coaster of ill health…, BMJ blog, 5 May 2020
https://blogs.bmj.com/bmj/2020/05/05/paul-garner-people-who-have-a-more-protracted-illness-need-help-to-understand-and-cope-with-the-constantly-shifting-bizarre-symptoms/
Hospitalisation: I never went to hospital, mainly because I wasn’t ill enough. We rang 111 on day 18 when things were bad, but by speaking to me they could tell my breathing difficulties weren’t enough to admit me. Perhaps this was good news, but I really wanted some medical expertise at this point. They took our details so a doctor could ring back to speak to me: the return call never came. My second 111 call on day 51 was similarly unhelpful (I’ll spare you the tale of the wasted hours on that call). My local GP was more accessible and supportive…
My local GP: Our local surgery in Stoke Newington was great, and they readily admitted they were still learning how to handle Covid-19 at this early stage. They rang me daily for a while during my worst spell. I think it’s good to be in contact with your GP, and see what they can do for you in your situation. On day 30 I was checked for oxygen levels and heart rate in the carpark behind the surgery (I shuffled slowly up the pavement with N for this rather bizarre but appreciated back-door appointment), and on day 54 I finally had a face-to-face meeting with my GP. They examined me thoroughly for secondary infections and sent links to two useful resources with details of recovery support from our local hospital and Covid 19-related research:
Post Covid-19 Patient Information Pack from Homerton University Hospital NHS Foundation Trust:
https://mcusercontent.com/30db5cb77411d59f467a2fecf/files/5fe19213-796d-4e9d-a04e-af9ab02c2acd/FYI_2_Post_COVID_19_information_pack.pdf
Oxford Covid -19 Evidence Service: regularly updated coronavirus evidence reviews, data analysis and writing:
http://www.cebm.net/oxford-covid-19-evidence-service/
Medication: It was paracetamol primarily. I became aware, through the support group, of other users taking medication (omeprazole) for silent reflux, which has similar symptoms to some related to Covid-19. I discussed this with my GP and started a four-week course of them on day 39, which helped. Compared to the cornucopia of medication some people obviously have taken, mine is small fry.
Crosswords, genealogy: sitting in the sun on a sofa turned to face out the front window, keeping still and calm, these two were a good balance of gentle and stimulating.
Things I didn’t do no.1: draw. I tried, but I just couldn’t do it. It was too much, and creativity dipped. I have a few bad unfinished drawings from this time. The first thing I was able to draw was my stubble.
Things I didn’t do no.2: read. I would fall asleep rather than read. American Marriage by Tayari Jones lay half read by my bed the whole time.
Things I didn’t do no.3: exercise. Over and over on the support group I would read about fit people recovering from the virus who resumed running 5km or even 10km at the first symptom-free day, and who then reported immediate relapses. I have taken short, gentle walks but no more.
News and media: I couldn’t bring myself to listen to news reports much - it fed anxiety, and I was aware that N and the girls would pick up on anything important and let me know. As much as anything, I needed to keep positive, and updates on the exponential growth of Covid-19 cases and deaths was not good for the mind.
Social media: I generally avoided it. I didn’t want to read about the wonderful creative opportunities that lockdown presented to us all, or badly researched medical stories too easily shared. I wanted useful practical information straight from the trusted expert source, although being so early on in the pandemic’s timeline even the most reliable sources were scrabbling around trying to get to grips with what we are dealing with. (That’s still true now, two months on as I write this.)
Reporting symptoms: Very early on I started reporting my symptoms on the world’s largest study of the virus, the Covid-19 Symptom Study app. Its website is good for essential Covid-19 reading and research.
Applauding the NHS every Thursday at 8pm: I recorded the second of these when things felt at their darkest for me. It was great to hear people whoop and holler in the buildings and streets around. N and the girls were in the windows below and or the doorstep joining in, not that I could see them. It was a great moment of connection early on, pre-Cummings, at a point when we really thought we were all in it together.
If you get Covid-19, it seems most likely you’ll get it mildly and recover quickly, or perhaps not even know you have had it. We all know that age, race, sex and other health issues play their parts in how seriously we get it. I expected, naively, that I would get through Covid-19 quite quickly. It didn’t turn out like that, as I have hinted. I am lucky that I have my family to support me through it all in ways I’ll never forget, that my employers are so understanding and supportive, and that, although it has stayed with me a long time, my own Covid-19 wasn’t serious enough to deliver me to intensive care. But of course you don’t know that when you’re going through it in the darkness, just as we don't know where it will lead us from here.
Most of all, stay well.
Published on June 01, 2020 07:21
No comments have been added yet.



