Karyn Hall's Blog
November 5, 2025
How Childhood Patterns Show Up in Adult Relationships
This week I’ve been thinking about relationships. Have you ever wondered why you keep dating the same type of person when it’s not working out for you? Or why certain fights with your partner feel familiar, even though you swore you’d never repeat your parents’ mistakes? Or maybe you find yourself behaving like your parents when you said you’d never do that?
��The truth is, your childhood experiences shape how you love, fight, trust, and connect as an adult. This isn’t about blaming your parents or dwelling on the past. It’s about understanding the patterns you learned early in life so you can make better choices now. You see, your brain is like a computer that got programmed in childhood. Those early programs still run in the background, affecting your relationships today. While others may have created the experiences that established these patterns for you, it’s up to you to change them. The good news? Once you spot these patterns, you can start to change them.
What Are Attachment Styles?
When you were a baby, you learned how relationships work by watching your caregivers. Were they consistent and loving? Did they ignore your needs? Were they unpredictable? Your brain took notes and created a blueprint for all future relationships.
These blueprints are called ��“attachment styles.” There are four main types:
Secure attachment:��Your caregivers were reliable and responsive. You learned that people are trustworthy and relationships are safe. As an adult, you’re comfortable with closeness and independence.
Anxious attachment:��Your caregivers were inconsistent, meaning sometimes loving, sometimes distant. You learned to worry about abandonment. As an adult, you might feel clingy, need constant reassurance, or fear being left.
Avoidant attachment:��Your caregivers were emotionally unavailable or dismissive. You learned to rely only on yourself. As an adult, you might struggle with intimacy, pull away when things get serious, or feel uncomfortable with emotions.
Disorganized attachment:��Your caregivers were frightening or chaotic. You learned that relationships are confusing and scary. As an adult, you might want closeness but push people away, or have dramatic, unstable relationships.
Most people aren’t purely one type���you might have different styles in different relationships or situations.
How Attachment Styles and Childhood Patterns Work Together
Understanding the connection between attachment styles and childhood patterns is important. They’re related but different:
Your attachment style��is the foundation���it’s the core belief system you developed about relationships. Think of it as your operating system that runs in the background.
Your childhood patterns��are the specific behaviors and coping strategies that grew from that foundation. These are like the apps running on your operating system.
Here’s how they connect:
From Anxious Attachment, you might develop:
The Anxious Pursuer pattern (constantly seeking reassurance)The Peacekeeper pattern (avoiding conflict to prevent abandonment)The Invisible Person pattern (believing your needs don’t matter enough to voice them)From Avoidant Attachment, you might develop:
The Emotional Wall pattern (keeping distance to feel safe)Strong independence that pushes people awayShutting down or leaving during conflictFrom Disorganized Attachment, you might develop:
The Recreating Chaos pattern (feeling comfortable with instability)Push-pull dynamics (wanting closeness but fearing it)The Fixer pattern (trying to control unpredictable situations by being needed)From Secure Attachment, you develop:
Healthy communication patternsComfort with both intimacy and independenceAbility to manage conflict constructivelyTwo people can have the same attachment style but show different patterns. For example, two people with anxious attachment might cope differently���one becomes a peacekeeper who avoids all conflict, while another becomes an anxious pursuer who needs constant contact. Same root cause, different survival strategies.
Your attachment style answers the question: “Do I fundamentally believe relationships are safe and people are trustworthy?”
Your childhood patterns answer: “What specific behaviors did I learn to cope with my attachment wounds?”
Understanding both helps you see the full picture of why you act the way you do in relationships.

Common Childhood Patterns That Follow You Into Adulthood
The Peacekeeper Pattern
What happened in childhood:��You grew up walking on eggshells. Maybe a parent had anger issues, struggled with addiction, or had unpredictable moods. You learned that your job was to keep everyone calm and happy.
How it shows up now:��You avoid conflict at all costs. You say “it’s fine” when it’s not fine. You apologize for things that aren’t your fault. You put everyone’s needs before your own, then feel resentful. You might even stay in bad relationships because leaving would cause conflict.
Why it’s a problem:��You lose yourself trying to manage other people’s emotions. Your needs don’t get met. Partners may take advantage of your people-pleasing, or they might feel frustrated because you never say what you really want.
The Anxious Pursuer Pattern
What happened in childhood:��Your parents’ love felt conditional or inconsistent. You had to work hard for attention and approval. Maybe they were emotionally distant, overly critical, or only showed love when you achieved something.
How it shows up now:��You need constant reassurance that your partner loves you. You panic when they don’t text back quickly. You analyze everything they say for hidden meanings. You might come on too strong early in relationships or feel anxious when you’re apart.
Why it’s a problem:��Your anxiety can push partners away, creating the exact abandonment you fear. You give away your power by making your worth dependent on someone else’s approval. You struggle to relax and enjoy relationships.
The Emotional Wall Pattern
What happened in childhood:��Showing emotions wasn’t safe. Maybe vulnerability was mocked, crying was punished, or expressing needs led to rejection. You learned to shut down your feelings and handle everything alone.
How it shows up now:��You have trouble opening up, even to people you love. You say “I don’t need anyone” and pride yourself on being independent. When conflict comes up, you shut down, leave the room, or go silent. Intimate conversations feel uncomfortable or scary.
Why it’s a problem:��Partners feel locked out and unloved. They can’t read your mind, so your needs don’t get met. Relationships stay surface-level and never deepen. You miss out on the closeness and support that make relationships meaningful.
The Fixer Pattern
What happened in childhood:��You had to grow up too fast. Maybe you took care of younger siblings, managed a parent’s emotions, or dealt with family problems that weren’t your responsibility. You learned your value comes from being helpful and needed.
How it shows up now:��You’re attracted to “projects”���people who need fixing. You give advice when people just want listening. You feel responsible for your partner’s happiness, problems, and growth. You struggle in relationships with healthy, stable people because you don’t feel needed.
Why it’s a problem:��You end up in one-sided relationships where you give everything and receive little. You enable unhealthy behavior by always rescuing people from consequences. You never learn to receive love���only to earn it through service.
The Recreating Chaos Pattern
What happened in childhood:��Your home life was dramatic, unstable, or chaotic. Even though it was painful, the intensity felt normal. Calm feels boring or uncomfortable because your nervous system is wired for crisis.
How it shows up now:��Healthy, stable relationships feel “boring.” You’re drawn to drama, intensity, and rollercoaster relationships. You might pick fights when things are going too well or mistake anxiety for passion. Calm partners don’t excite you.
Why it’s a problem:��You confuse toxicity with chemistry. You miss out on stable, loving relationships because they feel “wrong.” You exhaust yourself and your partners with constant drama. You never experience the peace and security that real love provides.
The Invisible Person Pattern
What happened in childhood:��Your needs were ignored, minimized, or dismissed. Maybe you had siblings who took all the attention, parents who were too busy, or a family where children were seen but not heard. You learned that your needs don’t matter.
How it shows up now:��You don’t ask for what you need. You feel guilty for having wants or taking up space. You’re surprised when partners ask about your day or care about your feelings. You might attract selfish partners because you don’t set boundaries.
Why it’s a problem:��You end up in relationships where you’re constantly giving but rarely receiving. You feel invisible and unimportant, confirming your childhood belief. Partners may not even know you’re unhappy because you never speak up.
How to Spot Your Patterns
Recognizing your patterns is the first step to changing them. Here are some questions to ask yourself:
What relationship behaviors do I keep repeating, even when they don’t work?What kind of people am I consistently attracted to?What situations in relationships trigger strong emotional reactions in me?What did I learn about love, conflict, and emotions from my family?What role did I play in my family (peacekeeper, caregiver, troublemaker, invisible one)?When do I feel most uncomfortable in relationships?Your answers reveal your patterns. Pay attention to repetitive themes in your relationships. If you keep having the same problems with different people, the common factor is you���and your childhood programming.
Breaking Free From Unhealthy Patterns
Awareness Is the Starting Point
You can’t change what you don’t recognize. Start noticing when old patterns show up. When you feel triggered, pause and ask: “Is this about now, or does this feel familiar from my past?”
For example, if your partner is 20 minutes late and you feel panicked about abandonment, that’s probably a childhood wound, not the current reality.
Challenge Your Automatic Thoughts
Your brain runs on old programming, creating automatic thoughts that feel true but might not be. Start questioning them.
Old thought: “If I express my needs, they’ll leave me.” Challenge: “Is this true, or is this what I learned as a child? Have people actually left when I’ve been honest?”
Old thought: “I have to fix everyone’s problems.” Challenge: “Is this my responsibility, or am I repeating a childhood role? What happens if I let people handle their own issues?”
Communicate Your Patterns to Your Partner
If you’re in a relationship, talk about your patterns. Say something like: “I realize I shut down during conflict because that’s what I learned growing up. I’m working on it, but I wanted you to understand why I do this.”
This creates understanding instead of blame. Your partner can support you rather than take your reactions personally.
Practice New Responses
Your brain forms new patterns through repetition. Each time you choose a different response, you weaken the old pattern and strengthen a new one.
If you’re a peacekeeper, practice saying “Actually, that doesn’t work for me” once a day. If you’re emotionally avoidant, practice sharing one feeling per day, even if it’s uncomfortable. If you’re anxious, practice sitting with the discomfort instead of immediately texting for reassurance.
Start small. You’re rewiring decades of programming���be patient with yourself.
Set Boundaries Based on Your Needs
Many childhood patterns involve ignoring your own needs to manage other people. Start identifying what you actually need in relationships and communicate those needs clearly.
“I need time alone to recharge���it’s not about you.” “I need you to listen without offering solutions right now.” “I need reassurance when I’m feeling insecure, even though I’m working on this.”
Good partners will respect reasonable boundaries. If they don’t, that’s important information.
Choose Different People
If your pattern is choosing emotionally unavailable people, start dating the person who seems “too nice.” If you pick projects, try someone who has their life together. If you want drama, give the stable person a chance.
This will feel weird at first. Your brain will tell you something is wrong because it doesn’t match your template. Push through the discomfort. Different isn’t wrong���it’s just unfamiliar.
What Healthy Relationships Actually Look Like
When you’ve only known unhealthy patterns, you might not recognize what healthy looks like. Here are some signs:
You feel safe expressing your needs and feelingsConflict gets resolved, not avoided or explodedYou can be yourself without fear of rejectionYour partner respects your boundariesYou feel secure without needing constant reassuranceYou have independence and togetherness in balanceTrust is the foundation, not jealousy or controlYou support each other’s growthLove feels peaceful, not chaoticHealthy might feel boring at first if you’re used to chaos. Give yourself time to adjust. Peace isn’t the same as boredom���it’s actually what safety feels like.
You’re Not Broken
If you see yourself in these patterns, that doesn’t mean you’re damaged or unlovable. It means you’re human. Every person brings their past into their present. The difference is whether you’re aware of it or not.
Your childhood patterns made sense in the environment you grew up in. They helped you survive. The problem is they’re not helping you anymore���they’re holding you back from the relationships you deserve.
You learned these patterns, which means you can unlearn them. It takes time, self-compassion, and consistent effort, but change is absolutely possible. Thousands of people have rewired their relationship patterns and built healthy, loving connections.
Your past doesn’t have to be your future. Understanding where your patterns come from gives you the power to choose something different. Start today, be patient with yourself, and remember: awareness is the first step to freedom.
Moving Forward
Change doesn’t happen overnight. You might slip back into old patterns, and that’s okay. Progress isn’t linear. Each time you recognize a pattern and choose differently, you’re building new neural pathways and creating a healthier relationship future.
Be gentle with yourself during this process. You’re not just changing behaviors���you’re healing old wounds and rewriting your story. That’s brave work.
You deserve relationships that feel safe, loving, and authentic. You deserve to be seen, heard, and valued. Your past shaped you, but it doesn’t define you. The relationships you create from here forward are up to you.
At the DBT Center, we are here to help. ��Call us at 713-973-2800
The post How Childhood Patterns Show Up in Adult Relationships appeared first on Houston DBT Center.
October 29, 2025
Practical Ideas for Helping with Burnout
Burnout has been on my mind. Each day feels filled with demands on our time, energy, and emotions. I want to share ideas on managing burnout and would love to hear what you do.
Understanding Burnout in the Real World
Burnout doesn���t care about vacation days or self-care routines. It appears when you juggle jobs, care for family, or struggle financially. The advice to “just take a break” feels out of touch when bills keep coming.
If you feel chronic exhaustion, cynicism about your work, or emotional depletion, you���re likely facing burnout. If you���re reading this, you probably can���t step away completely.
Why Traditional Burnout Advice Falls Short
Most burnout recovery advice assumes some privilege: take a sabbatical, quit a toxic job, or book a spa weekend. But what you can’t do that? What if you���re a single parent working two jobs? What if you care for aging parents while building your career? Or if your finances make leaving impossible? Many facing burnout can’t escape their situations. This doesn���t always mean negative circumstances. It could be an overload of positive demands. Recovery is still possible; it just needs different strategies.

Micro-Recovery: Small Actions with Real Impact
When you can’t take extended time off, focus on micro-recovery moments throughout your day. These brief interventions can interrupt the stress cycle and provide genuine relief. Aim for 1 to 5 minutes every hour. Try really enjoying a sip of coffee, for example. Sound meaningless? ��Science says it makes a difference through the following:
Sensory shift: The aroma, warmth, and flavor of coffee engage your senses, providing a distinct shift away from your ongoig��visual and mental input.Mindfulness practice: Focusing on the repetitive, calming motion of sipping and the simple pleasure of the beverage acts as a grounding exercise. This helps unwind your tension.Physical movement: The simple act of getting up to make the coffee counteracts the effects of prolonged sitting, improving circulation and reducing physical tension.Intentional pause: Unlike simply scrolling through a phone during a break, which still engages the brain, the process of making and enjoying coffee is an intentional act of stepping away that signals a true mental reset. Plus you don’t have the potential upsetting input of social media content!Restores focus. The brain can only sustain attention for a certain period of time before it starts to decline. A short break can renew your alertness.Reduces Cortisol Levels. If you can distract yourself for a few minutes and relax your body, cortisol levels can decrease which is super important for your health but also how wound up you feel inside.
Morning boundaries: Before checking your phone or email, spend five minutes doing something just for you. Stretch, drink coffee in silence, or step outside. This creates a buffer between rest and responsibility. If you do something you enjoy, it can shift your mindset from negative (energy draining) thoughts that you hate getting out of bed. ��Give yourself something that you look forward to in the mornings.
Evening transitions: Create a 10-minute ritual between work and home life. Change clothes, take a walk around the block, take a shower, or listen to a specific playlist. This signals to your brain that you’re shifting modes, even if you’re working from home.
��Weekend protection: Guard at least one morning or afternoon on weekends as non-negotiable personal time. Even three hours of protected space can provide meaningful recovery. ��Do something you enjoy. Watching television often isn’t as relaxing as it is numbing. If you do watch TV, try to find something active like laughing out loud or playing along with a gameshow.
Energy Management Over Time Management
When you’re burned out and can’t reduce your workload, shift your focus from managing time to managing energy. Not all tasks drain you equally, and not all hours are created equal. Notice how much energy you might be putting into routine tasks that can be done with much less energy.
��Identify your energy patterns:��Track when you feel most alert and capable versus depleted. Schedule your most demanding tasks during high-energy windows and administrative work during low-energy periods.
Batch similar tasks:��Group similar activities together to reduce the mental switching cost. Answer all emails in one block, make all phone calls in another, and protect creative work time separately.
��Use the “good enough” standard:��Perfectionism accelerates burnout. For tasks that don’t truly matter, consciously choose “good enough” over excellent. Save your best energy for what genuinely counts.
��Automate and eliminate: Identify tasks you can automate, delegate, or stop doing entirely. Every unnecessary task you eliminate creates space for recovery, even if it’s small. ��Look for ways that you may be wasting your time or your energy or both.
Building Sustainable Boundaries in Unsustainable Situations
You might not be able to leave your situation, but you can still set boundaries within it. Boundaries aren’t about saying no to everything���they’re about protecting your core capacity. Do you really need to add another page to the proposal? ��Do you really need to volunteer to provide treats for an event? ��Say no to extras.
Practice selective availability with work:��You don’t have to be responsive 24/7. Set specific times when you check messages and communicate this to others. Even a one-hour communication blackout can provide relief.
Reframe obligations:��Not every request is equally urgent. Use the��Eisenhower Matrix��to separate what’s truly urgent and important from what simply feels that way. Many “urgent” demands can actually wait. ��Also, be aware of when you are responding with urgency that doesn’t actually help the response be any faster, it just drains your energy and stresses you more.
Protect your off time:��When you’re not working, really be off. Set up auto-responders, turn off notifications, or use separate devices for work and personal life if possible.
The Power of Micro-Self-Care
Self-care doesn’t require money, time, or elaborate planning. When resources are limited, focus on accessible acts of care that require minimal investment. What can you do in 5 or 10 minutes, or maybe 20, that really helps you feel more relaxed or more positive?
Sleep protection:��Guard your sleep fiercely, as much as possible. Keep consistent sleep and wake times, limit screens an hour before bed, and create the darkest, coolest sleeping environment possible. Sleep is the foundation of burnout recovery.
Movement as medicine:��You don’t need a gym membership or an hour to exercise. Five minutes of stretching, dancing to one song, or walking around your building counts. Movement interrupts stress hormones and boosts mood-regulating chemicals. Walking in nature is one of the best stress relievers. Focus on the nature, not what’s on your to-do list.
Connection in small doses:��Burnout thrives in isolation. Send one text to a friend, have a brief conversation with a neighbor, or participate in online communities. Even small connections combat the loneliness that intensifies burnout.
Nourishment without perfection:��When exhausted, we often skip meals or grab whatever’s quick. Keeping simple, nourishing options available���protein bars, pre-cut vegetables, frozen fruit���ensures you’re fueling your body even when cooking feels impossible.
Managing the Emotional Weight of Burnout
Burnout isn’t just physical exhaustion���it’s emotional depletion. When you can’t change your circumstances immediately, managing your emotional response becomes crucial.
Acknowledge the reality:Stop pretending you’re fine or blaming yourself for struggling. Your situation is genuinely difficult. Acknowledging this without judgment can relieve the additional burden of toxic positivity.Grieve what you’re missing:It’s okay to feel sad, angry, or resentful about needing to work this hard or having limited options. Give yourself permission to feel these emotions rather than suppressing them.Find meaning where possible:Even in difficult circumstances, connecting to purpose helps. Remind yourself why you’re doing this���whether it’s providing for family, working toward a goal, or simply surviving. Meaning sustains us when motivation fades.Practice self-compassion:Talk to yourself the way you’d talk to a friend in this situation. Replace “I should be handling this better” with “I’m doing the best I can in a difficult situation.”Remember the positive:��Make a list of what is going right, what you’re grateful for. It’s easy to forget the positive. It’s not about denying the stress, but it’s about seeing the full picture.Creating a Long-Term Exit Strategy
While managing burnout in place, simultaneously work on an exit strategy, even if it takes years. Small steps toward change compound over time.
Financial preparation:Even saving $10 per paycheck creates options. Build an emergency fund, reduce expenses where possible, or explore additional income streams that require minimal time investment.Skills development:Use microlearning opportunities���podcasts during commutes, free online courses, or certification programs���to build skills that create future opportunities.Network quietly:Maintain professional connections, update your resume periodically, and keep aware of opportunities even if you’re not actively searching. When the time comes to transition, you’ll be ready.Document:Keep records of your accomplishments, build your portfolio, and gather references. Future you will thank present you for this preparation.
Finding Hope in Difficult Circumstances
Managing burnout when you can’t take a break isn’t about pretending everything is fine or powering through indefinitely. It’s about survival, strategy, and self-preservation while you navigate difficult circumstances.
Your situation might not change overnight, but every small action you take to protect your wellbeing matters. Micro-recoveries accumulate. Boundaries compound. Small acts of self-care add up.
You’re not failing because you’re burned out in a situation you can’t immediately leave. You’re surviving something genuinely difficult, and that takes tremendous strength. Be gentle with yourself as you navigate this, and remember that this chapter won’t last forever.
Remember:��If you’re experiencing severe burnout symptoms, reach out for professional support. You don’t have to navigate this alone, and asking for help is a sign of strength, not weakness.
The post Practical Ideas for Helping with Burnout appeared first on Houston DBT Center.
October 27, 2025
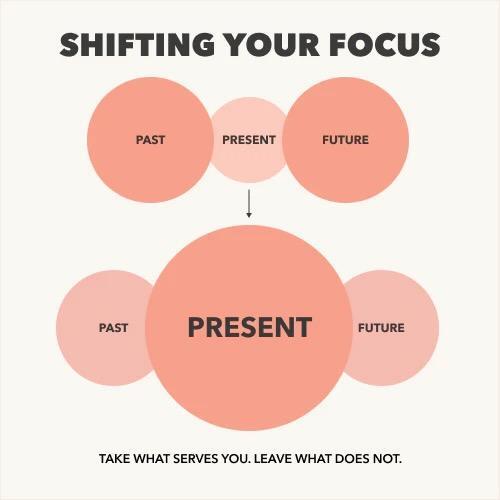
Balance Past, Present & Future with DBT and RODBT
Most of us spend a lot of time in our minds��� time machine���replaying the past, worrying about the future, and missing the only place we can truly live: the present moment. It���s natural to want to understand what went wrong yesterday or to plan for what���s coming next week, but getting stuck there can create suffering. Worrying about the future often brings anxiety. Being focused on the past can bring resentment, bitterness, or ongoing sadness. At the Houston DBT Center, we help clients learn how to balance reflection, presence, and preparation using principles from Dialectical Behavior Therapy (DBT), Mindfulness, and Radically Open DBT (RO DBT).
When Your Mind Keeps Time TravelingOur brains are designed to remember and to anticipate. Remembering helps us learn; anticipating helps us prepare. Being in the present though is where we need to be to live. Spending too much time in the past or the future��can keep us trapped.
Replaying the past can lead to regret, shame, or endless ���if-only��� thinking.
Living in the future can create anxiety, over-control, and constant pressure to be ready for every possibility.
Living in the present connects us to what���s real���our senses, relationships, and purpose���but takes mindful effort.
The key is to hold both truths: the past and future matter, and the present is where change happens.
 DBT: Balancing Acceptance and Change
DBT: Balancing Acceptance and ChangeDialectical Behavior Therapy (DBT) was developed to help people find balance between acceptance and change. That same principle applies to how we hold time.
Acceptance means acknowledging what has happened, even if we wish it were different.
Change means using that awareness to make wiser choices now and for the future.
DBT teaches core skills that support this balance:
Mindfulness skills bring awareness to when your mind drifts into rumination or worry.
Distress tolerance helps you stay grounded when memories or fears feel intense and there is no learning or planning, It just pulls you out of the present
Emotion regulation teaches you to respond effectively to feelings tied to both past experiences and future concerns.
Through practice, you begin to live from Wise Mind ���that balanced space where emotion and reason meet, and where you can take effective action in the moment. ��Accepting what can’t be changed (doesn’t mean you like it) and working to change what you can.
 Mindfulness: Returning Home to Now
Mindfulness: Returning Home to NowMindfulness is the practice of noticing where your attention goes and gently guiding it back to the present. It���s not about emptying your mind���it���s about becoming aware.
You might notice:
When you���re replaying a conversation or anticipating one.
How your body feels right now���your breath, posture, or surroundings.
What���s happening in this moment that you can actually influence or appreciate.
Each time you return to now, you strengthen the part of your brain that helps regulate emotions, reduce anxiety, and build calm focus. Mindfulness therapy at our Houston center helps clients learn simple practices that fit daily life���from pausing between meetings to breathing before a difficult discussion.
��RO DBT: Flexibility, Openness, and Letting Go of Control
Radically Open DBT (RO DBT) addresses��what happens when we try to controltoo much���over-analyzing the past or over-planning the future.
People who are highly conscientious, perfectionistic, or rule-focused often feel safest when everything is planned and predictable. But constant control can limit connection, spontaneity, and joy.
RO DBT teaches:
Openness to experience, even when uncertainty feels uncomfortable.
Social signaling skills���showing warmth, receptivity, and trust to others.
Self-enquiry, a gentle curiosity about understanding ��the cause for what we do instead of rigid self-criticism.
By loosening perfectionism and cultivating flexibility, clients rediscover a sense of aliveness���able to plan wisely without missing what���s happening now.
Integrating the Past, Present, and FutureBalance doesn���t mean giving each equal time; it means knowing when to shift focus.
Reflect on the past to learn, not to punish yourself.
Plan for the future to prepare, not to prevent all discomfort.
Stay in the present to live, not to escape responsibility.
When we learn to carry the past and future lightly, we become more engaged, compassionate, and resilient in the present.
Living the Dialectic: Fully Present, Gently ForwardAt the Houston DBT Center, our therapists use DBT and ��RO DBT to help clients find this equilibrium���whether you struggle with anxiety, perfectionism, trauma, or emotional over-control.
Each approach teaches a version of the same truth:
The only place you can change your life is right here, right now.
You can honor your past, plan for your future, and still live fully today.
That���s the essence of balance���and of psychological freedom.
We provide evidence-based therapy in Houston and online throughout Texas, including DBT, RO DBT, and Mindfulness-based approaches for adults, teens, and families.
To learn more or schedule an intake, call 713-973-2800 or visit www.houstondbtcenter.com.
The post Balance Past, Present & Future with DBT and RODBT appeared first on Houston DBT Center.
October 8, 2025
Early Intervention with Sand Tray Therapy
s a parent, you naturally watch for signs your child is healthy and thriving. But while we’re quick to notice a fever or scraped knee, recognizing mental health struggles in young children can feel much harder. Is this just a phase? Am I overreacting? When should I actually seek help?
If you’re asking these questions, you’re not alone. Many parents struggle to know when typical childhood emotions cross into concerning territory. This guide will help you recognize mental health warning signs in young children and understand how early intervention���including powerful therapeutic approaches like sand tray therapy���can make a lasting difference.
Why Early Mental Health Intervention Matters for Your ChildEarly childhood mental health intervention refers to professional support for children (typically ages 2-8) experiencing emotional, behavioral, or psychological challenges. The earlier these concerns are addressed, the better your child’s long-term outcomes.
Here’s why timing matters: Your child’s brain is developing rapidly during these early years. Neural pathways are forming that will influence how they handle stress, regulate emotions, and navigate relationships throughout life. Mental health support during this critical window can literally reshape brain development in positive ways.
Research shows that children who receive early mental health intervention experience:
Better emotional regulation and coping skillsImproved relationships with family and peersGreater school readiness and academic successReduced risk of mental health problems in adolescence and adulthoodStronger resilience when facing future challengesThe good news? Young children are remarkably responsive to treatment. What might become a deeply ingrained pattern later can often be addressed more easily when caught early.
Mental Health Red Flags: When to Seek Help for Your ChildEvery child has bad days, tantrums, and fears���these are normal parts of development. But certain patterns signal that your child needs professional support. Trust your parental instincts, and watch for these warning signs.
Childhood Anxiety SymptomsNormal childhood fears (like being scared of the dark) are different from anxiety disorders in children. Seek help if your child shows:
Separation anxiety ��that persists beyond age 5 or worsens over timeExtreme distress about attending preschool or daycare, even after months of adjustmentPhysical complaints (stomachaches, headaches) with no medical cause, especially before school or social eventsConstant worry about everyday situations (what if the car breaks down, what if you forget to pick me up)Avoidance of age-appropriate activities they previously enjoyedDifficulty sleeping due to fears or worryExcessive need for reassurance (“Are you sure nothing bad will happen?”)Panic attacks in children (rapid heartbeat, difficulty breathing, overwhelming fear)Depression in Young ChildrenYes, preschool depression and childhood depression are real. Watch for:
Persistent sadness or irritability lasting two weeks or longerLoss of interest in playing, friends, or favorite activitiesChanges in energy (either lethargy or agitation)Frequent crying or emotional meltdownsSelf-criticism unusual for their age (“I’m bad,” “Nobody likes me”)Withdrawal from family and friendsConcerning statements about wanting to disappear or not wanting to existChanges in appetite or sleep patternsTrauma Symptoms in ChildrenChildhood trauma��from abuse, neglect, violence, frightening medical procedures, natural disasters, or loss requires immediate attention. Trauma symptoms in young children include:
Nightmares, night terrors, or sleep problemsRepetitive trauma play���reenacting scary experiences through play over and overBeing constantly on edge or easily startledRegression (acting like a younger child, bedwetting after being potty-trained)Increased aggression or sudden fearfulnessSeeming emotionally “flat” or detachedPTSD in children (flashbacks, avoidance, hypervigilance)Behavioral and Emotional Regulation ProblemsWhile tantrums are developmentally normal for toddlers, certain patterns need attention:
Frequent, intense tantrums beyond age 4Aggression that endangers the child or others regularlyEmotional dysregulation���inability to calm down even with parental supportExtreme reactions that seem way out of proportionDifficulty transitioning between activities without major meltdownsOppositional defiant behavior that disrupts family functioningImpulsive behaviors that create safety concernsTrouble understanding social cues or others’ emotionsWhen Your Gut Says Something’s WrongHere’s the most important guideline: If you’re consistently worried about your child’s emotional wellbeing, that concern deserves professional attention. You know your child better than anyone. Trust yourself.
Don’t wait for problems to become severe. Early assessment either provides reassurance or opens the door to helpful support���it’s a win either way.
 What Is Sand Tray Therapy? A Powerful Tool for Children’s Mental Health
What Is Sand Tray Therapy? A Powerful Tool for Children’s Mental HealthSand tray therapy for children (also called sandplay therapy) is a specialized form of play therapy that’s incredibly effective for young children struggling with mental health issues. If your child’s therapist recommends this approach, here’s what you need to know.
How Sand Tray Therapy WorksImagine a shallow box filled with sand and hundreds of miniature figures���people, animals, houses, trees, vehicles, monsters, bridges, fences, and more. In sand tray therapy, your child uses these materials to create scenes in the sand that represent their inner world.
There are no rules about what to create or how to play. The child has complete freedom. They might:
Build elaborate worlds with clear storiesCreate abstract designs or patternsStage battles, rescues, or everyday scenariosBury objects, build mountains, dig riversPlace figures carefully or change scenes repeatedlyThe child therapist observes closely but lets your child lead. This isn’t about talking through problems���it’s about giving form to feelings and experiences that are too big, scary, or confusing for words.
Why Sand Tray Therapy Is Perfect for Young ChildrenYoung children think concretely and communicate naturally through play. Child psychology research confirms that children process experiences and emotions differently than adults. Their language centers are still developing, but their emotional brains are fully active.
Sand tray therapy meets children where they are developmentally:
Play is children’s natural language. When kids play, they’re not just having fun���they’re working through experiences, testing ideas, and making sense of their world. Sand tray therapy harnesses this innate process for healing.
No talking required. A four-year-old with anxiety may not know how to explain the tight feeling in their chest. But they can show a small animal surrounded by bigger, scary ones. The symbolic play communicates what words cannot.
Safe distance from scary stuff. The miniature figures let children explore difficult experiences without confronting them directly. A traumatized child might stage a car crash with toy vehicles, processing the event at a comfortable psychological distance.
Sensory and calming. The sand itself is therapeutic. Its texture is naturally regulating for many children. The ability to shape and transform it provides a sense of control���powerful medicine for kids who feel powerless.
Mastery through repetition. Children naturally repeat experiences they’re working to understand. A child might create similar scenes session after session, gradually changing details as they process and heal.
What Can Sand Tray Therapy Treat?Sand tray therapy has strong research support and clinical evidence for treating:
Childhood anxiety disorders (separation anxiety, generalized anxiety, specific phobias, social anxiety)Childhood trauma and PTSD (abuse, neglect, witnessing violence, medical trauma, natural disasters)Depression in children and griefBehavioral problems (aggression, defiance, impulsivity)Emotional regulation difficultiesSocial-emotional challenges and relationship problemsStress from family transitions (divorce, new siblings, moves)Selective mutism and communication difficultiesWhat to Expect from Sand Tray Therapy SessionsSessions typically last 45-50 minutes and follow a gentle, child-led structure:
1. Your child chooses figures and creates a scene. The therapist provides the materials and a safe, non-judgmental space. Your child has complete freedom to create whatever they wish.
2. The therapist observes and sometimes asks gentle questions. They might say, “Tell me about this part” or “What’s happening here?” But they never criticize, correct, or direct the play.
3. Your child shares if they want to. Some kids narrate their entire process. Others work silently. Both are fine. The act of creating is therapeutic even without verbal explanation.
4. The therapist documents the tray (usually with photos) to track themes and progress over time.
5. Your child dismantles the scene (or the therapist does after the session), returning to a blank slate for next time.
Seeing Progress in the SandOver multiple sessions, healing becomes visible in the trays themselves. Early sessions might show:
Chaos, with figures scattered randomlyViolence, crashes, or scary scenariosSeparation themes or trapped figuresEmpty trays or minimal engagementAs therapy progresses, trays often shift toward:
More organization and structureProtective elements (fences, safe houses, helper figures)Resolution of conflicts within the scenePeaceful coexistence of previously threatening elementsMore integrated, cohesive scenesThese changes in play reflect internal changes in your child’s emotional world. The chaos they felt inside is becoming more organized. The overwhelming feelings are becoming manageable.
Many therapists integrate multiple methods based on your child’s needs. The best approach is whatever helps your child feel safe and engaged.
��What About Therapy for Parents?Parent coaching or family therapy often accompanies child therapy. Your child’s therapist may:
Teach you strategies for supporting your child at homeHelp you understand what your child is working throughAddress family dynamics that impact your child’s wellbeingProvide education about childhood mental healthYour involvement matters tremendously. The most effective treatment happens when therapy room and home reinforce each other.
Questions Parents Ask About Sand Tray TherapyWill I be in the room during sessions?
Usually no. Children express themselves more freely without parental presence. Your therapist will provide updates about progress.
What if my child creates violent or scary scenes?
This is actually common and therapeutic. Children use play to work through difficult material. Trained therapists know the difference between healthy processing and concerning content.
How long does sand tray therapy take?
It varies. Some children show improvement in 8-12 weeks; others benefit from longer-term support. Your therapist will discuss goals and timeline.
Does sand tray therapy really work?
Yes. Research supports its effectiveness, and many parents report remarkable changes in their children’s emotional regulation, anxiety levels, and behavior.
Is my child too young (or too old) for sand tray therapy?
Sand tray therapy works well for ages 3-12, though approaches vary by age. Younger children use it more freely; older children (and adults) might combine it with talk therapy.
Call us at 713-973-2800 if you are interested in play therapy/sand tray therapy.����
The post Early Intervention with Sand Tray Therapy appeared first on Houston DBT Center.
October 2, 2025
DBT for Borderline Personality Disorder
Borderline Personality Disorder (BPD) is a complex mental health condition that affects how people think, feel, and connect in relationships. Individuals with BPD often struggle with intense emotions, impulsive behaviors, self-harm, or fears of abandonment. These challenges can feel overwhelming for both the individual and their loved ones. Fortunately, Dialectical Behavior Therapy (DBT) is one of the most effective, research-based treatments available for BPD.
Let’s explore how DBT works, why it���s considered the gold standard for BPD, and how programs such as DBT Intensive Outpatient Programs (IOP) offer a structured alternative to hospitalization.
What Is Borderline Personality Disorder?Borderline Personality Disorder impacts approximately 1.6% of the population, though some studies suggest it may be higher. Common symptoms include:
Intense, rapidly shifting emotions
Fear of abandonment
Self-harm or suicidal behaviors
Unstable or chaotic relationships
Impulsive or risky behaviors
Chronic feelings of emptiness
Left untreated, BPD can significantly impact daily life. However, with the right treatment, recovery and stability are possible.
Learn more about BPD from the National Institute of Mental Health.
 What Is DBT?
What Is DBT?Dialectical Behavior Therapy (DBT) was developed by Dr. Marsha Linehan specifically to treat individuals with chronic suicidality and borderline personality disorder. DBT combines cognitive behavioral therapy (CBT) techniques with mindfulness practices to help individuals regulate emotions, reduce harmful behaviors, and build healthier relationships.
DBT focuses on four core skill areas:
Mindfulness ��� learning to stay grounded in the present moment.
Distress Tolerance ��� coping with crisis situations without making them worse.
Emotion Regulation ��� understanding and managing intense emotions.
Interpersonal Effectiveness ��� building healthier, more stable relationships.
These skills give clients practical tools to replace self-destructive behaviors with healthier coping strategies.
For an overview of DBT, see the American Psychological Association.
��Why DBT Works for Borderline Personality DisorderResearch consistently shows that DBT is one of the most effective treatments for BPD. Studies have found DBT reduces:
Frequency and severity of self-harm behaviors
Suicide attempts
Hospitalizations
Emergency room visits
At the same time, DBT improves:
Emotion regulation
Relationship stability
Overall quality of life
A 2014 study published in JAMA Psychiatry found that DBT significantly reduced suicide attempts compared to other treatment approaches (source).
��DBT IOP: An Alternative to HospitalizationWhen someone with BPD experiences severe symptoms, hospitalization is often considered. However, repeated or extended hospital stays can sometimes be disruptive and may not provide the skills needed for long-term stability. In fact, research has shown that for individuals with BPD, frequent hospitalization can be associated with poorer outcomes (Paris, 2004).
That���s where a DBT Intensive Outpatient Program (IOP) comes in.
DBT IOP provides the intensity of care often needed during crisis without removing individuals from their daily lives. Clients attend multiple sessions each week, including:
DBT skills groups
Individual therapy
Skills coaching between sessions
This structured, supportive environment helps clients build the skills to manage emotions and relationships while staying connected to work, school, and family.
��DBT and BPD: Hope and HealingLiving with borderline personality disorder can feel overwhelming, but it���s important to know that effective treatment exists. DBT offers a pathway to healing, helping individuals replace destructive patterns with healthier coping tools and more fulfilling relationships.
If you or a loved one is struggling with symptoms of BPD, seeking out a qualified DBT program���such as a local outpatient or intensive outpatient program���can be life-changing.
At the Houston DBT Center, our experienced clinicians offer comprehensive DBT programs for teens and adults. We are committed to providing evidence-based, compassionate care that supports lasting recovery.
713-973-2800
The post DBT for Borderline Personality Disorder appeared first on Houston DBT Center.
September 17, 2025
Can Eating Disorders Be Treated Without Inpatient Care?
The answer is yes. When people think of eating disorder treatment, they often imagine long hospital stays or residential programs, away from their homes and families. For some this can get in the way of seeking treatment. No doubt about it, while inpatient care can be life-saving in medical or crisis situations,��not every individual with an eating disorder requires inpatient treatment. For many teens and adults, outpatient options like an��Intensive Outpatient Programs (IOP)���combined with a supportive treatment team���can provide effective, compassionate care while allowing clients to continue with school, work, and daily life.
When Is Inpatient Care Necessary?
Inpatient or residential programs are typically recommended when:
Medical stability is at risk (dangerously low weight, heart issues, electrolyte imbalances).A person is unable to maintain safety without 24-hour support.Previous outpatient attempts with treatments for complex eating disorders have not been effective.In these situations, 24-hour monitoring ensures that both the physical and psychological risks of an eating disorder are addressed.

The Role of Outpatient & IOP Treatment
For individuals who are medically stable but still struggling with eating disorder thoughts and behaviors,��outpatient therapy or an IOP can be highly effective and allows the individual to remain with friends and family members and learn coping skills that meet the needs of their everyday life. Outpatient programs can be created to fit the needs of the client.
Standard Outpatient
Standard outpatient treatment is typically one individual session a week, and possibly a skills or other group. This can often be effective for mild eating disorder symptoms.
What Is an Intensive Outpatient Program (IOP)?
When you think of an IOP you may think about groups meeting for several hours a day, often 2 or 3, for multiple days a week. But an IOP can be multiple sessions of individual therapy or multiple individual sessions, a family session, and a group session. An IOP provides structured, evidence-based treatment several days per week, usually in the afternoons or evenings. At Houston DBT Center, our IOP is flexible and depends on the needs of the client
Individual Sessions:�� to work on personal goals and coping strategies.
May be DBT or RO DBT, or may focus on a specific treatment such as CBT for anxiety.
Group therapy sessions��using DBT and RO DBT, , and other evidence-based approaches.
Individual therapy��to work on personal goals and coping strategies.Family support and education, which research shows significantly improves recovery outcomes..
Where to Start: Building a Treatment Team
A key part of successful outpatient eating disorder care is creating a��collaborative treatment team. At the DBT Center we will work with you to build your team:�� This often includes:
Therapist specializing in eating disorders (DBT, RO DBT, CBT-E).Dietitian/Nutritionist��experienced in eating disorder recovery and nutrition rehabilitation.Medical provider��(primary care doctor or psychiatrist) to monitor physical health and medications if needed.Family members or trusted supports, included in therapy when appropriate.Client with their values and goalsThis team works together to address the physical, emotional, and relational aspects of the eating disorder���providing��comprehensive care without requiring inpatient hospitalization. They will work with you to help you build your treatment plan.
Therapist
A psychotherapist plays a central role in eating disorder treatment by helping clients understand and change the psychological and behavioral patterns that keep the disorder going. While medical providers and dietitians focus on physical health and nutrition stabilization, the therapist works with the emotional, cognitive, and relational aspects of the illness. They create a safe space for clients to explore underlying issues such as perfectionism, shame, trauma, or difficulties with emotional regulation, all of which can fuel disordered eating behaviors.
Therapists also provide evidence-based treatments���such as Dialectical Behavior Therapy (DBT), Radically Open DBT (RO DBT), Cognitive Behavioral Therapy for Eating Disorders (CBT-E), or Family-Based Treatment (FBT)���depending on the client���s needs. These approaches help individuals identify and challenge distorted thoughts about food, body image, and self-worth, while also teaching coping skills to manage urges, regulate emotions, and build healthier relationships.
Another key part of a psychotherapist���s work is coordination with the treatment team. Eating disorder recovery often requires collaboration with physicians, psychiatrists, and dietitians. The therapist communicates with these providers to ensure consistent care and to monitor risks, such as medical instability or suicidality.
Finally, psychotherapists support families or loved ones who may be struggling to understand how to help. In family or couples sessions, they teach validation, communication, and boundary-setting skills, and provide education about the disorder. This relational work is especially important for adolescents, where parental involvement can significantly improve outcomes.
Nutritionists
Registered dietitians and nutritionists who take part in your treatment can help you learn more about your eating disorder and create a plan to regain and maintain healthy eating habits. It’s important to seek treatment from someone who has specialized training in eating disorders because this training is not standard for dietitians. Goals of nutrition education may be to:
Work toward a healthy weight for your personal history and body type.Learn how nutrition affects your body, including knowing how your eating disorder causes nutrition issues and physical problems.Practice eating flexibly and with sufficient portions to support health and development.Set consistent eating patterns ��� generally, at least three meals a day with at least one to two snacks.Correct health problems due to poor nutrition.Challenge food phobias and/or mythsMedical Professionals
In eating disorder treatment, a medical doctor (MD) plays an essential role in keeping recovery safe and supported. Because eating disorders can impact the entire body���including the heart, digestive system, hormones, and bones���regular medical check-ins are a key part of treatment. Even when someone doesn���t ���look sick,��� eating disorders can cause serious health problems that aren���t visible on the outside.
The doctor���s role is to monitor physical health and make sure your body is stable enough to focus on recovery. This may include checking vital signs, reviewing lab work, tracking weight changes, and looking for complications such as dehydration or nutrient imbalances. If a higher level of care is ever needed, the doctor helps determine when inpatient or residential treatment might be the safest option.
Your doctor also works closely with the rest of your treatment team���including therapists, dietitians, and sometimes psychiatrists���so that every part of your recovery is covered. They may adjust medications, answer medical questions, and provide education for both you and your family about how eating disorders affect the body.
In short, the MD is there to make sure your health is protected while you do the important emotional and nutritional healing in therapy and dietitian sessions. This team approach allows you to move toward recovery with both safety and support.
You, the Client
In eating disorder treatment, the client is not just a recipient of care���they are an active and vital member of the treatment team. Recovery is most effective when clients are engaged in the process and see themselves as partners alongside their therapist, medical doctor, dietitian, and other providers.
The client���s role includes being honest about thoughts, feelings, and behaviors, even when it feels difficult or uncomfortable. This openness helps the treatment team understand what is really going on and tailor support in the most helpful way. Clients are encouraged to share what���s working, what feels overwhelming, and what goals matter most to them. Their voice is central in shaping the direction of treatment.
Another important part of the client���s role is practicing new skills and strategies outside of sessions. Therapy offers tools for managing emotions, challenging unhelpful thoughts, and improving relationships with food and body. But real change happens when those skills are applied in daily life, meal by meal, choice by choice. Even small steps forward are meaningful progress.
Clients also play a role in self-advocacy and collaboration. This might mean asking questions, setting boundaries, or working with the team to adjust treatment plans as recovery evolves. By actively participating, the client builds self-trust and strengthens a sense of ownership over their healing journey.
Most importantly, the client brings courage and commitment to the process. While the treatment team provides guidance, expertise, and support, the client is the one who ultimately does the brave work of recovery���reclaiming health, freedom, and hope for the future.
Families
In outpatient eating disorder treatment, families play a crucial role in supporting recovery. Eating disorders don���t just affect the individual���they often impact the entire family system. When families are included in treatment, recovery tends to be stronger and more sustainable, especially for children, teens, and young adults living at home.
The family���s role begins with creating a safe, supportive home environment. This might mean helping with meal support, reducing diet talk at home, and encouraging balanced routines around rest, activity, and self-care. Families can also help by learning about eating disorders, so they understand that the illness is not a choice and recovery takes time, patience, and compassion.
At the Houston DBT Center, families may be invited to participate in therapy sessions, depending on the needs of the client. These meetings provide a space to improve communication, strengthen validation skills, and learn how to respond effectively to the challenges of recovery. Parents or partners often work closely with therapists and dietitians to practice skills that reduce conflict and increase support during meals and daily life.
Another important family role is consistency. Recovery can bring ups and downs, and it���s normal for clients to feel ambivalent about change. Families who remain steady, compassionate, and firm in their support help keep treatment on track.
Ultimately, families are partners in healing. By showing up with empathy, patience, and willingness to learn, loved ones help create the kind of environment where lasting recovery is possible.
Benefits of Outpatient & IOP Care
Remain connected to daily routines and responsibilities.Learn and practice recovery skills in real-life situations.Involve family members or partners more easily in treatment.More flexible and cost-effective compared to residential care.For many clients, IOP combined with a strong treatment team offers the��right balance of support and independence.
Finding the Right Level of Care
Every eating disorder is unique, and treatment should be tailored to the individual. At Houston DBT Center, we begin with a careful assessment to recommend the most effective level of care���whether that���s outpatient therapy, IOP, or referral to a higher level of support.
Recovery is possible. With the right care, many people can heal from an eating disorder��without inpatient treatment, while still receiving the structure and expertise they need.
Are you ready? ��Call us at 713-973-2800.
The post Can Eating Disorders Be Treated Without Inpatient Care? appeared first on Houston DBT Center.
September 10, 2025
Ca Eating Disorders Be Treated Without Inpatient Care?
The answer is yes. When people think of eating disorder treatment, they often imagine long hospital stays or residential programs, away from their homes and families. For some this can get in the way of seeking treatment. No doubt about it, while inpatient care can be life-saving in medical or crisis situations,��not every individual with an eating disorder requires inpatient treatment. For many teens and adults, outpatient options like an��Intensive Outpatient Programs (IOP)���combined with a supportive treatment team���can provide effective, compassionate care while allowing clients to continue with school, work, and daily life.
When Is Inpatient Care Necessary?
Inpatient or residential programs are typically recommended when:
Medical stability is at risk (dangerously low weight, heart issues, electrolyte imbalances).A person is unable to maintain safety without 24-hour support.Previous outpatient attempts with treatments for complex eating disorders have not been effective.In these situations, 24-hour monitoring ensures that both the physical and psychological risks of an eating disorder are addressed.
The Role of Outpatient & IOP Treatment
For individuals who are medically stable but still struggling with eating disorder thoughts and behaviors,��outpatient therapy or an IOP can be highly effective and allows the individual to remain with friends and family members and learn coping skills that meet the needs of their everyday life. Outpatient programs can be created to fit the needs of the client.
Standard Outpatient
Standard outpatient treatment is typically one individual session a week, and possibly a skills or other group. This can often be effective for mild eating disorder symptoms.
What Is an Intensive Outpatient Program (IOP)?
When you think of an IOP you may think about groups meeting for several hours a day, often 2 or 3, for multiple days a week. But an IOP can be multiple sessions of individual therapy or multiple individual sessions, a family session, and a group session. An IOP provides structured, evidence-based treatment several days per week, usually in the afternoons or evenings. At Houston DBT Center, our IOP for ED is flexible and depends on the needs of the client
��Individual Sessions:�� to work on personal goals and coping strategies. May be DBT or RO DBT, or may focus on a specific treatment such as CBT for anxiety.
Group therapy sessions��using DBT and RO DBT, , and other evidence-based approaches.
Individual therapy��to work on personal goals and coping strategies.Family support and education, which research shows significantly improves recovery outcomes.
Where to Start: Building a Treatment Team
A key part of successful outpatient eating disorder care is creating a��collaborative treatment team. At the DBT Center we will work with you to build your team:�� This often includes:
Therapist specializing in eating disorders (DBT, RO DBT, CBT-E).Dietitian/Nutritionist��experienced in eating disorder recovery and nutrition rehabilitation.Medical provider��(primary care doctor or psychiatrist) to monitor physical health and medications if needed.Family members or trusted supports, included in therapy when appropriate.Client with their values and goalsThis team works together to address the physical, emotional, and relational aspects of the eating disorder���providing��comprehensive care without requiring inpatient hospitalization. They will work with you to help you build your treatment plan.
Therapist
A psychotherapist plays a central role in eating disorder treatment by helping clients understand and change the psychological and behavioral patterns that keep the disorder going. While medical providers and dietitians focus on physical health and nutrition stabilization, the therapist works with the emotional, cognitive, and relational aspects of the illness. They create a safe space for clients to explore underlying issues such as perfectionism, shame, trauma, or difficulties with emotional regulation, all of which can fuel disordered eating behaviors.
Therapists also provide evidence-based treatments���such as Dialectical Behavior Therapy (DBT), Radically Open DBT (RO DBT), Cognitive Behavioral Therapy for Eating Disorders (CBT-E), or Family-Based Treatment (FBT)���depending on the client���s needs. These approaches help individuals identify and challenge distorted thoughts about food, body image, and self-worth, while also teaching coping skills to manage urges, regulate emotions, and build healthier relationships.
Another key part of a psychotherapist���s work is coordination with the treatment team. Eating disorder recovery often requires collaboration with physicians, psychiatrists, and dietitians. The therapist communicates with these providers to ensure consistent care and to monitor risks, such as medical instability or suicidality.
Finally, psychotherapists support families or loved ones who may be struggling to understand how to help. In family or couples sessions, they teach validation, communication, and boundary-setting skills, and provide education about the disorder. This relational work is especially important for adolescents, where parental involvement can significantly improve outcomes.
Nutritionists
Registered dietitians and nutritionists who take part in your treatment can help you learn more about your eating disorder and create a plan to regain and maintain healthy eating habits. It’s important to seek treatment from someone who has specialized training in eating disorders because this training is not standard for dietitians. Goals of nutrition education may be to:
Work toward a healthy weight for your personal history and body type.Learn how nutrition affects your body, including knowing how your eating disorder causes nutrition issues and physical problems.Practice eating flexibly and with sufficient portions to support health and development.Set consistent eating patterns ��� generally, at least three meals a day with at least one to two snacks.Correct health problems due to poor nutrition.Challenge food phobias and/or mythsMedical Professionals
In eating disorder treatment, a medical doctor (MD) plays an essential role in keeping recovery safe and supported. Because eating disorders can impact the entire body���including the heart, digestive system, hormones, and bones���regular medical check-ins are a key part of treatment. Even when someone doesn���t ���look sick,��� eating disorders can cause serious health problems that aren���t visible on the outside.
The doctor���s role is to monitor physical health and make sure your body is stable enough to focus on recovery. This may include checking vital signs, reviewing lab work, tracking weight changes, and looking for complications such as dehydration or nutrient imbalances. If a higher level of care is ever needed, the doctor helps determine when inpatient or residential treatment might be the safest option.
Your doctor also works closely with the rest of your treatment team���including therapists, dietitians, and sometimes psychiatrists���so that every part of your recovery is covered. They may adjust medications, answer medical questions, and provide education for both you and your family about how eating disorders affect the body.
In short, the MD is there to make sure your health is protected while you do the important emotional and nutritional healing in therapy and dietitian sessions. This team approach allows you to move toward recovery with both safety and support.
You, the Client
In eating disorder treatment, the client is not just a recipient of care���they are an active and vital member of the treatment team. Recovery is most effective when clients are engaged in the process and see themselves as partners alongside their therapist, medical doctor, dietitian, and other providers.
The client���s role includes being honest about thoughts, feelings, and behaviors, even when it feels difficult or uncomfortable. This openness helps the treatment team understand what is really going on and tailor support in the most helpful way. Clients are encouraged to share what���s working, what feels overwhelming, and what goals matter most to them. Their voice is central in shaping the direction of treatment.
Another important part of the client���s role is practicing new skills and strategies outside of sessions. Therapy offers tools for managing emotions, challenging unhelpful thoughts, and improving relationships with food and body. But real change happens when those skills are applied in daily life, meal by meal, choice by choice. Even small steps forward are meaningful progress.
Clients also play a role in self-advocacy and collaboration. This might mean asking questions, setting boundaries, or working with the team to adjust treatment plans as recovery evolves. By actively participating, the client builds self-trust and strengthens a sense of ownership over their healing journey.
Most importantly, the client brings courage and commitment to the process. While the treatment team provides guidance, expertise, and support, the client is the one who ultimately does the brave work of recovery���reclaiming health, freedom, and hope for the future.
Families
In outpatient eating disorder treatment, families play a crucial role in supporting recovery. Eating disorders don���t just affect the individual���they often impact the entire family system. When families are included in treatment, recovery tends to be stronger and more sustainable, especially for children, teens, and young adults living at home.
The family���s role begins with creating a safe, supportive home environment. This might mean helping with meal support, reducing diet talk at home, and encouraging balanced routines around rest, activity, and self-care. Families can also help by learning about eating disorders, so they understand that the illness is not a choice and recovery takes time, patience, and compassion.
At the Houston DBT Center, families may be invited to participate in therapy sessions, depending on the needs of the client. These meetings provide a space to improve communication, strengthen validation skills, and learn how to respond effectively to the challenges of recovery. Parents or partners often work closely with therapists and dietitians to practice skills that reduce conflict and increase support during meals and daily life.
Another important family role is consistency. Recovery can bring ups and downs, and it���s normal for clients to feel ambivalent about change. Families who remain steady, compassionate, and firm in their support help keep treatment on track.
Ultimately, families are partners in healing. By showing up with empathy, patience, and willingness to learn, loved ones help create the kind of environment where lasting recovery is possible.
Benefits of Outpatient & IOP Care
Remain connected to daily routines and responsibilities.Learn and practice recovery skills in real-life situations.Involve family members or partners more easily in treatment.More flexible and cost-effective compared to residential care.For many clients, IOP combined with a strong treatment team offers the��right balance of support and independence.
Finding the Right Level of Care
Every eating disorder is unique, and treatment should be tailored to the individual. At Houston DBT Center, we begin with a careful assessment to recommend the most effective level of care���whether that���s outpatient therapy, IOP, or referral to a higher level of support.
Recovery is possible. With the right care, many people can heal from an eating disorder without inpatient treatment, while still receiving the structure and expertise they need. ��Are you ready? ��Call us at 713-973-2800.
The post Ca Eating Disorders Be Treated Without Inpatient Care? appeared first on Houston DBT Center.
Loving Your Perfectionism: Don’t “Fix” It-Find a Balance
Perfectionism often carries a heavy reputation. It���s frequently linked with stress, anxiety, and burnout���but the truth is, perfectionism isn���t all bad. In fact, loving your perfectionism can mean embracing its strengths while learning to soften its edges. By understanding both the positives and negatives, you can find a healthier balance and use your perfectionism to thrive.
The Positives of PerfectionismPerfectionism can fuel incredible achievements. Many of the qualities tied to perfectionism are the same traits that lead people to excel in academics, careers, and creative pursuits.
Strengths of perfectionism include:
High standards: Striving for excellence often results in high-quality work.
Persistence: Perfectionists rarely give up, showing determination even in difficult situations.
Attention to detail: Precision can help avoid mistakes and deliver exceptional results.
Reliability: Others often see perfectionists as dependable and conscientious.
Research has shown that conscientiousness and striving for achievement are strongly associated with positive outcomes in education and career success (American Psychological Association).
When balanced well, these traits become assets���not burdens.
The Negatives of PerfectionismThe other side of perfectionism, however, can take a toll on mental and physical health.
Challenges of perfectionism include:
Self-criticism: High standards can easily turn into harsh self-judgment.
Fear of failure: Perfectionists may avoid risks, fearing they won���t meet expectations.
Burnout: Overworking to ���get it right��� can lead to exhaustion.
Strained relationships: Constant focus on flaws (in self or others) can create tension.
Perfectionism Paralysis: Stuck because you fear you can’t do it or be good enoughPerfectionism has been linked to anxiety, depression, eating disorders, and other mental health challenges (National Library of Medicine). Left unchecked, it can prevent people from enjoying life and embracing imperfection.
 Finding Balance: Loving Your Perfectionism Without Letting It Rule You
Finding Balance: Loving Your Perfectionism Without Letting It Rule YouThe key isn���t to eliminate perfectionism���it���s to love it in balance. You can keep its strengths while loosening its grip on your happiness.
Strategies for balance:
Practice self-compassion: Learn to treat yourself with the same kindness you���d offer a friend. Dr. Kristin Neff���s work offers excellent tools.
Set flexible goals: Aim high, but allow room for mistakes and growth.
Celebrate progress, not just results: Shift focus from ���perfect outcomes��� to effort and learning.
Check your inner dialogue: Replace critical thoughts with supportive reminders.
Seek support if needed: Therapy approaches like Dialectical Behavior Therapy (DBT) and Radically Open DBT (RO-DBT) can help perfectionists build self-acceptance and resilience (Behavioral Tech).
Loving the Whole PictureLoving your perfectionism means recognizing that it���s part of you���but not all of you. It���s about embracing the motivation and dedication it gives you, while gently addressing the rigidity and self-criticism it can bring.
When you learn to balance your perfectionist traits, you free yourself to enjoy both success and peace of mind. Striving for excellence and loving yourself���imperfections included���can coexist beautifully.
If your perfectionism has become maladaptive, the goal isn’t to “fix” it. The goal is to have a balance so that perfectionism works for you and not against your mental health and joy in life.
If you want help with your perfectionism, call us at 713-973-2800. We offer IOP and regular outpatient options.��
The post Loving Your Perfectionism: Don’t “Fix” It-Find a Balance appeared first on Houston DBT Center.
September 3, 2025
How Fears of Abandonment Show Up in BPD
One of the hardest parts of living with Borderline Personality Disorder (BPD) is the deep fear of being abandoned or left behind. For someone with BPD, even small things���like a friend canceling plans, a partner not answering a text quickly, or a loved one seeming distracted���can feel terrifying.
This fear is not just a little worry. It feels overwhelming and painful, and it often leads to behaviors that can be confusing to others. Let���s look at how fear of abandonment shows up, why it happens, and how Dialectical Behavior Therapy (DBT) can help.
��Why Fear of Abandonment Happens in BPDThe official definition of BPD (from the DSM-5-TR) includes ���frantic efforts to avoid abandonment.��� This means that people with BPD often do whatever they can, including extreme behaviors, to stop people from leaving.
This isn���t about being ���clingy��� or ���dramatic.��� For someone with BPD, the fear of abandonment feels real and intense, like their whole sense of safety depends on it. Their brain reacts as if being left behind is an emergency, a life or death crisis.
Behaviors Caused by Fear of AbandonmentFear of abandonment can show up in many different ways. Here are some common behaviors:
Needing constant reassurance
Sending lots of texts or calls to check in.
Asking, ���Do you really love me?��� again and again.
Pushing people away before they leave
Breaking up suddenly.
Starting fights to protect themselves from being hurt.
Ups and downs in relationships
One minute believing someone is perfect, the next minute thinking they don���t care at all.
Big reactions to small separations
Feeling panicked if a partner is late.
Melting down if plans change.
Testing loyalty
Picking fights or creating situations to ���see if the person will stay.���
Self-harm or threats
Sometimes, when fear feels unbearable, the person may hurt themselves or threaten to as a way to show their pain or keep someone close.
Example: Maria���s StoryMaria, age 26, loved her partner deeply. When he didn���t answer her text for several hours, Maria started to panic. She felt sure he didn���t care anymore. She sent dozens of messages, accused him of pulling away, and then threatened to leave the relationship herself. Later, when he reassured her, Maria felt ashamed and afraid he might actually leave for good.
��This cycle is common with BPD. It makes relationships like a rollercoaster. Fear of being left drives behaviors that can actually push people away, which then makes the fear even stronger.
 How DBT Helps With Fear of Abandonment
How DBT Helps With Fear of AbandonmentThe good news is that there is a treatment that works. Dialectical Behavior Therapy (DBT) is the most effective therapy for BPD (Behavioral Tech).
DBT Outpatient TreatmentOutpatient DBT usually includes:
Weekly individual therapy to work on specific struggles, like abandonment fears.
Weekly skills group to learn coping skills.
Phone coaching to get help in the moment when emotions feel too big.
DBT Intensive Outpatient Program (IOP)A DBT IOP is a more structured program for people who need extra support. It usually includes:
Several DBT groups each week.
Individual therapy.
A safe space to practice skills with others who understand.
DBT teaches skills that help with abandonment fears, including:
Mindfulness: staying in the present instead of spinning into fear.
Distress tolerance: calming down without acting on impulse.
Interpersonal effectiveness: asking for closeness or support without pushing people away.
Emotion regulation: learning how to lower the intensity of anger, panic, or despair.
Building Healthier RelationshipsWith DBT, people with BPD can learn to understand their fears and handle them in healthier ways. Instead of panic, fights, or self-harm, they can learn to ask for support, trust others, and feel more secure in relationships.
At the Houston DBT Center, we offer both outpatient DBT and DBT IOP programs. We help people with BPD face abandonment fears, build coping skills, and create stronger, more stable relationships.
ConclusionFear of abandonment is painful���but with the right treatment, it doesn���t have to control your life. DBT helps people with BPD break the cycle of fear and learn healthier ways to connect with others. Healing is possible, and stability in relationships can become a reality.
The post How Fears of Abandonment Show Up in BPD appeared first on Houston DBT Center.
September 2, 2025
Comprehensive Eating Disorder Treatment for Teens and Adults at the Houston DBT Center
By Karyn Hall, Ph.D., Founder
At the��Houston DBT Center, we offer specialized treatment for��adolescents and adults struggling with eating disorders, including��anorexia nervosa,��bulimia nervosa,��binge eating disorder,��compulsive overeating, and��orthorexia.
Our eating disorders treatment is included as part of treating a wide variety of diagnoses. Providing eating disorder treatment in a setting that includes individuals with a variety of mental health concerns, rather than limiting care to groups made up only of those with eating disorders, offers unique benefits for recovery. A mixed-diagnosis environment allows clients to hear different perspectives and learn from a wide range of coping skills, which can broaden insight and foster hope. It helps reduce the risk of a person���s identity becoming centered solely on the eating disorder, supporting a more well-rounded sense of self. Exposure to peers navigating different challenges can also encourage cognitive flexibility, empathy, and openness���qualities that are essential for long-term change. Moreover, the therapeutic skills taught in these settings, such as managing emotions, tolerating distress, and improving relationships, are applicable across all diagnoses, creating a dynamic learning space that better reflects the diversity of situations clients will face in everyday life.
Our evidence-based, level-based care ensures each individual and family get the right level of support at the right time while continuing with their individual therapist.We work closely with��adults, teens and their families��to address the complex emotional, behavioral, and relational factors that contribute to disordered eating. From outpatient care to more intensive support, our program is built around treatments proven to help you recover, including��Family-Based Treatment (FBT),��Cognitive Behavioral Therapy for Eating Disorders (CBT-E),��Exposure and Response Prevention (ERP),��Dialectical Behavior Therapy (DBT), and��Radically Open DBT (RO DBT).

Assessment
At the��Houston DBT Center, an eating disorder assessment��is the first step toward lasting recovery. Whether you are concerned about��anorexia nervosa,��bulimia nervosa,��binge eating disorder,��ARFID,��orthorexia, or another eating-related concern, our goal is to understand your unique experience so we can create a treatment plan tailored to your needs.
What to Expect During Your Assessment
Our evaluation process helps us identify the nature of the eating disorder, any co-occurring conditions, and the safest and most effective level of care. This includes:
Clinical Interview����� We listen to your story, exploring current symptoms, eating patterns, body image concerns, medical history, and important life circumstances.Standardized Screening Tools����� We use evidence-based questionnaires to assess eating disorder symptoms, mood, anxiety, personality style, and related mental health concerns.Medical and Nutritional Review����� With your consent, we coordinate with your medical provider and, when needed, a registered dietitian to address physical health and nutritional needs.Risk and Safety Evaluation����� We assess for any urgent medical complications, suicidal thoughts, or self-harming behaviors to determine if��outpatient therapy or intensive outpatient (IOP) is indicated. If residential care is needed, we will refer you to trusted facilities.Strengths and Goals����� We identify what matters most to you so your��eating disorder treatment plan��reflects your values and supports long-term recovery.Why a Comprehensive Assessment Matters
An accurate assessment is essential for��diagnosing eating disorders��and guiding effective treatment. Many individuals with eating disorders also experience��anxiety,��depression,��obsessive-compulsive disorder (OCD), or��personality-related coping styles��that influence recovery. Understanding the full picture allows us to recommend the right combination of therapies���such as��Dialectical Behavior Therapy (DBT),��Radically Open DBT (RO DBT),��Cognitive Behavioral Therapy for Eating Disorders (CBT-E),��Family-Based Treatment (FBT), or��Exposure and Response Prevention (ERP)���to help you heal both body and mind.
At the Houston DBT Center, our assessment process is not about judgment���it is about listening deeply, providing compassionate support, and building a clear plan for your recovery journey.
[image error]Our Level-Based Approach to Treating Eating Disorders
We start with the least intensive level of care that can be effective, based on an assessment of needs, and level up support only when needed. This often allows you to stay involved in treatment while minimizing disruption to school, work, and daily life.
Teens
Most younger teens begin treatment with weekly individual sessions and family sessions, where Family-Based Treatment (FBT), the gold standard for adolescents with anorexia or bulimia, is indicated. In FBT, parents are the main support for helping their teen eat regular meals and restore health. If regular outpatient treatment is not enough, or families need more structure, we offer skills classes that address coping needs for the teen. We also have an IOP for a more intensive treatment. When needed, we include a nutritionist who specializes in ED and a medical professional to manage and oversee physical health needs.
Even as teens move into more intensive treatment,��families remain a central part of the healing process. Parents receive coaching on how to support eating at home and learn to apply FBT principles during key meals. At the same time, teens continue working on their recovery through daily CBT-E sessions and targeted group support.
For older teens, weekly individual sessions and group sessions are often the starting point, in either RO DBT or DBT.
Adults
Adults may begin their recovery with an individual weekly session. Depending on the need, it could be an individual session and a group skills session weekly. We can add additional individual sessions or IOP if needed. We have the flexibility to create a program that fits your needs.
ERP
We also integrate��ERP (Exposure and Response Prevention)��when indicated to help adults and teens face food-related fears and anxieties. This approach is especially effective for teens and adults ��who also struggle with��OCD or anxiety disorders, both of which commonly occur with eating disorders. ERP helps individuals learn that they can tolerate distress, eat more flexibly, and reduce fear-based rituals around food.
��

Individual Therapy for Eating Disorders: CBT-E
In addition to family therapy, teens and adults ��in our program can receive��Enhanced Cognitive Behavioral Therapy (CBT-E). CBT-E helps teens:
Identify unhelpful thoughts about body image, food, and weightUnderstand how these thoughts affect their behavior and emotionsLearn healthier patterns of thinking and copingCBT-E is especially effective for treating��the over-evaluation of body shape and weight���a core feature of many eating disorders. This tendency to base self-worth on appearance can lead to intense anxiety, perfectionism, and isolation. CBT-E gives tools to challenge these beliefs and build a healthier identity.
Advanced Treatment Options: DBT and RO DBT Tracks
Some teens and adults benefit from extra support for��underlying personality traits��that maintain their eating disorder. That���s why we offer two specialized therapy tracks as part of our higher levels of care:
Our��DBT Track��helps teens and adults who struggle with��emotion dysregulation��and��impulsivity���traits often seen in those who binge eat, purge, or self-harm. DBT teaches skills to:
Manage intense emotionsCope with distress in healthy waysImprove relationshipsReduce impulsive or self-destructive behaviorThrough a structured program of��mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness, DBT supports you in building a life worth living and sharing.

Radically Open DBT (RO DBT)
What is RO DBT?
RO DBT is transdiagnostic evidenced-based therapy developed by Dr. Thomas Lynch. RO DBT targets disorders of over-control, such as certain eating disorders. It focuses on building connections and reducing an internal sense of loneliness and isolation, which underlies many disorders.
Our��RO DBT Track��is designed for those who tend to be��overcontrolled. These are individuals who may appear “fine” on the outside but suffer quietly with:
Social withdrawalExcessive self-control or rigidityLoneliness or perfectionismDifficulty expressing emotionsRO DBT focuses on increasing openness, emotional expression, and connection with others. It helps you become more flexible, spontaneous, and socially engaged���what we call ���rejoining the tribe.��� This treatment is especially helpful for those with anorexia or orthorexia who find it hard to let go of control.
Returning to Outpatient Care with Ongoing Support
As you make progress in our IOP (either adult or teen), you can transition back to��weekly therapy where they continue practicing the skills they���ve learned. Because our approach is��fully integrated, teens and families work with the same individual therapist throughout the process, ensuring��continuity of care��and a smoother return to everyday life.
��
Why Choose the Houston DBT Center?
At the Houston DBT Center, we are committed to:
Evidence-based treatment��rooted in the latest researchPersonalized care��tailored your needsFamily involvement��for teensSupport for co-occurring conditions, such as anxiety, OCD, or traumaA compassionate, experienced team of cliniciansGet Help Today
If you or your teen is struggling with an eating disorder, early intervention makes a difference.
������Contact us today at 713-973-2800��to schedule an intake or learn more about our eating disorder treatment programs. You can email us at administration@dbtcenterhouston.com
The post Comprehensive Eating Disorder Treatment for Teens and Adults at the Houston DBT Center appeared first on Houston DBT Center.



