Nancy Kay's Blog
February 23, 2026
Temperament Testing in Dogs
Let’s say you want to adopt a puppy from a litter of ten. How will you decide which one to bring home? Based on gender, color, or markings? Based on how sleepy or active or smitten with you they appear during your brief visit? How can you confidently choose which one will be the right fit for you and your household?
 Photo by Laura Roberts on UnsplashTemperament Testing
Photo by Laura Roberts on UnsplashTemperament TestingThe best way to predict the adult behavior of young puppies is through temperament testing. This assessment is best performed on 7-week-old pups (give or take a little bit) by someone with temperament testing experience.
Speaking for Spot - Dr. Nancy Kay is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
Pups are exposed to various situations and are scored based on their confidence level, social behavior, desire for play, and reactions to play stimuli, prey stimuli, loud noise, and separation.
Here’s a fun video of temperament testing on a litter of beagle puppies.
Looking for a chill family dog, a long-distance running partner, a hunting dog? Results of temperament testing can help guide you.
Temperament Testing Based on SalivaA study published earlier this month on adult dogs documented that the amount of cortisol (a stress hormone) and serotonin (a feel-good hormone) in their saliva correlated with behavior patterns.
Concentrations of salivary cortisol and serotonin were measured in 24 dogs before and after standardized temperament testing. Findings showed that the dogs with higher stress reactivity, based on temperament testing, had higher cortisol levels. Serotonin levels were increased in those with greater emotional regulation (stability).
This study has a very small sample size (24 dogs) and I look forward to results of more studies to validate these findings. I wonder if, some day, such testing might be practical enough to allow shelters to better match dogs with their forever homes.
Have you had experience with temperament testing? If so, did you (do you) find it helpful? I’d love for all my dog trainer/behaviorist readers to chime in.
Best wishes to you and your four-legged family members for abundant good health,
Dr. Nancy
DrNancyKay.com
Speaking for Spot - Dr. Nancy Kay is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
February 16, 2026
What a Dog's Nose Knows
With about 220 million scent receptors, dogs have a sense of smell that we mere mortals, with only five million receptors, can fathom. Their noses are powerful enough to detect a single drop of a liquid smell in 20 combined Olympic-size swimming pools!
 Photo by Pancrazio Auteri on Unsplash
Photo by Pancrazio Auteri on UnsplashDogs who who have a knack for scent training can perform so many tremendous functions for their sensory-challenged human counterparts. We’ve all seen working dogs used to detect a variety of smells: narcotics, explosives, lost people and animals, wildlife, people buried under rubble, and cadavers
Speaking for Spot - Dr. Nancy Kay is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
Here are some other things dogs can be trained to sniff out:
Truffle HuntingDo you love the taste of truffles? If so, you may have a dog to thank for this. The most popular truffle hunting dog breed is the Lagotto Romagnolo. Originally bred in Italy to be duck hunting dogs, their natural truffle hunting prowess has become far more profitable. They sniff the forest floor and dig in the mud to expose this mushroom delicacy.
 Lagotto Romagnolo Photo by Stephen Kidd on UnsplashLow Blood Sugar Detection
Lagotto Romagnolo Photo by Stephen Kidd on UnsplashLow Blood Sugar DetectionCheck out the National Institute of Canine Service and Training (formerly Dogs4Diabetics) a nonprofit organization in Vacaville, California. Here experts scent train dogs (some collected from local shelters) to partner with insulin-dependent diabetics. When the dogs detect odors associated a low blood sugar, they alert their humans with a nudge or nose poke, pawing or scratching, or even jumping, face-licking, or vocalizing.
Too much insulin can cause hypoglycemia (low blood sugar), a potentially dangerous and even life threatening situation. A common fear among insulin-dependent diabetics is that their blood sugar might drop to a dangerously low level while they’re asleep. Imagine the peace of mind provided by a 24-hour scent trained companion.
Human CancersA variety of studies have documented the ability of scent trained dogs to detect some human cancers:
melanoma (skin cancer)
colorectal cancer
ovarian cancer
breast cancer
prostate cancer
lung cancer
These dogs can aid in early disease detection, which can result in a better outcome.
Canine HemangiosarcomaHemangiosarcoma is a common malignant canine cancer that arises from vascular (blood vessel) cells. Hemangiosarcoma likes to set up housekeeping in middle-aged to older large breed dogs where it usually grows undetected, often within the spleen or liver. Acute severe symptoms arise when the tumor “springs a leak” with massive blood loss into the abdomen.
Emergency surgery can stop the bleeding, but by the time the crisis arises, the long-term prognosis is grim.
A new study from the University of Pennsylvania has documented that dogs can be scent-trained to positively identify hemangiosarcoma. This work is in its infancy, but does offer promise for early detection of this cancer in the future.
BedbugsI’ve never experienced bedbugs up close and personal, nor do I want to, but I hear they’re bloody awful! Scent detection dogs can scan a room for the presence of bedbugs in minutes and target the exact locations of the infestation. This is far more efficient than visual inspection of the room and dismantling of furniture.
Take a look at this fun video.
Parkinson’s DiseaseWithout highly specialized testing, Parkinson’s disease can be difficult to diagnose. A two-year study of 23 scent-trained dogs documented a keen ability to differentiate Parkinsonian from non-Parkinsonian patients. Imagine the diagnostic benefit this can provide.
SeizuresResearch has shown that dogs can learn to detect scent changes prior to an epileptic seizure. Because of the dog’s alert, the affected person can seek safety by sitting on the floor, stopping the car, putting a baby down, calling for help, etc.
Not all dogs have the disposition and scent capabilities to become scent-trained service dogs. Whether or not your dog has the potential to become a “pro,” scent-training can be a fun activity to share.
What unique sniffing capabilities does your dog have—nasty old tennis balls, animal bones, cat poop, fish carcasses?
Best wishes to you and your four-legged family members for abundant good health,
Dr. Nancy
DrNancyKay.com
Speaking for Spot - Dr. Nancy Kay is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
February 9, 2026
Now More Than Ever, We Need Our Dogs
Now more than ever, we need all the sweetness, joy, and unconditional love our dogs can provide. They’re good medicine for counteracting the fear, anger, sadness, and helplessness many of us are feeling.
 Photo by Anushka Sharma on Unsplash
Photo by Anushka Sharma on UnsplashPlenty of evidence substantiates the positive impact dogs have on our mental health.
Speaking for Spot - Dr. Nancy Kay is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
A study out of the United Kingdom found that students who watched videos of dogs experienced significant mood improvement and decreased anxiety. Those who interacted directly with a dog experienced an even greater decline in anxiety and improved mood scores.
A Canadian study documented that therapy dogs lessened pain, anxiety, and depression for emergency room patients and improved their overall sense of well being.
In 2023, the American Psychiatric Association published a poll of 2,200 Americans. 87% of those with dogs reported that their four-legged companion had a positive impact on their mental health by providing unconditional love and support, companionship, and acting as a calming presence.
Johns Hopkins reports that petting a dog increases blood levels of the feel-good hormones serotonin and dopamine.
What if you don’t have a dog?But what if you’d like an intravenous infusion of doggie dopamine, but don’t have a dog? No problem. Here are some options for you:
Watch some of the shenanigans that go on at your local dog park. If I were a psychotherapist, I’d prescribe visits to the dog park for my clients with depression. I really would!
Foster a dog from a local shelter, pound, or rescue organization. Fostering dogs until they’re adopted not only helps you, it helps make these animals far more adoptable and frees up kennel space for other dogs. Be forewarned, “foster failures” are common—you can’t give up the foster who has captured your heart. Perhaps we should rename them “foster wins!”
Become a puppy raiser with a nonprofit such as Guide Dogs for the Blind or Canine Companions for Independence. A NYT article discussed the fact that nonprofits such as these are facing a dramatic shortage of volunteers, creating 2-4 year long wait times for service dogs.
Humane societies and animal shelters have an endless need for people to help with feeding, grooming, and walking dogs. Some allow you to take a dog for a day. Why not volunteer?
How does your dog provide you with emotional support?
Best wishes to you and your four-legged family members for abundant good health,
Dr. Nancy
DrNancyKay.com
Speaking for Spot - Dr. Nancy Kay is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
February 2, 2026
Clients Veterinarians Wish They Could Clone
Just as teachers have their “pet students,” so too do veterinarians have their “pet clients” (no pun intended). These are the clients who generate a buzz of excitement amongst the veterinary staff whenever their names appear in the appointment schedule. They have a knack for making the job of caring for their pets such a pleasure.
 Photo by sarah b on Unsplash
Photo by sarah b on UnsplashLet’s call our “red carpet client” Jasmine. What is it about Jasmine that elicits such enthusiasm from the vet clinic staff? Here are some of her endearing characteristics:
Speaking for Spot - Dr. Nancy Kay is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
She arrives well preparedJasmine knows the brand name of the food she feeds her dog (not just the color of the bag), and she brings in a list of all his medications and supplements, including the dosage schedule. She can accurately report on her dog’s medical progress such as frequency of vomiting or how many seizures as he had since his last appointment.
She’s informedLike most of us, Jasmine checks in with Dr. Google and AI about medical issues. But she knows how to surf responsibly, following the recommendations provided in a previous blog post. She doesn’t waste anyone’s time on ridiculous notions and anecdotal information.
Before the office visit, Jasmine prepares a list of questions, but holds off asking them until the veterinarian has had the chance to ask her own questions, perform a physical exam, and discuss her findings.
She provides her undivided attentionJasmine silences her phone and has arranged supervision of impulsive youngsters to avoid distraction during the office visit.
She follows the game planJasmine arrives on time for her appointment, not only out of respect for the veterinary staff, but for the other “on deck”clients in the waiting room.
She does her absolute best to follow doc’s orders for things such as administering medications, restricting calories, and calling in with progress reports. If Jasmine has a question or concern about the agreed upon plan, she contacts her vet rather than revising the plan on her own.
Jasmine brings her animals in for annual checkups, even when there are no health concerns or vaccinations due.
She’s respectful and appreciativeThe entire veterinary staff receives sincere respect and appreciation from Jasmine. She understands that it’s the receptionist who decides whether or not to squeeze in an urgent request to be seen at 5:00 on a Friday afternoon. She’s aware that the technicians care for hospitalized patients, sterilize surgical equipment, monitor anesthesia, and so much more, and that the kennel assistants disinfect all the surfaces that could be breeding grounds for contagious diseases.
Along with expressing her gratitude verbally, Jasmine sends thank-you notes and holiday greetings cards, and from time to time, she delivers yummy treats for the staff to enjoy.
She discusses her concernsAs difficult as it can sometimes be, Jasmine shares her concerns, such as about cost or a recommended test or medication, with her veterinarian. She knows that, besides caring about her patients, her vet cares deeply about the emotional well-being of her clients.
What kinds of things do you do that make the veterinary staff happy to see you?
Dr. Nancy
drnancykay.com
Speaking for Spot - Dr. Nancy Kay is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
January 26, 2026
Rapamycin: A Fountain of Youth for Dogs?
Veterinary medicine is constantly advancing, and three drugs in the limelight right now are rapamycin, potassium bromide, and Laverdia.
RapamycinThe Dog Aging Project is one-of-a-kind research hoping to identify, explain, and slow the aging process. The results may provide some insights into human longevity. To date, approximately 50,000 dogs of all sizes, breeds, and ages are enrolled in the study.
Speaking for Spot - Dr. Nancy Kay is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
 Photo by Walter van Zyl on Unsplash
Photo by Walter van Zyl on UnsplashOne part of the Dog Aging Project is called TRIAD (Test of Rapamycin in Aging Dogs).
Rapamycin is an antibiotic shown to extend the lifespan of mice by 9-20%. Its use in people is a hot topic, even though there’s no hard and fast evidence that it helps people live longer. Longevity guru, Dr. Peter Attia, often discusses the use of rapamycin on his podcast.
The Dog Aging Project is currently recruiting participation in their TRIAD study. Want to enroll your dog? You can if your dog meets certain criteria and you live near a study site location.
I look forward to the results of this study!
Potassium bromideOral anti-seizure medications are the mainstay of successful treatment of canine epilepsy. One of these medications is potassium bromide which, until recently, has only been available as an oral liquid with a horribly bitter taste. Many dogs are unwilling to take it.
The FDA (Food and Drug Administration) has just approved a formulation of potassium bromide that is a tablet that will be much easier to administer. If you’ve been battling with your dog to take potassium bromide, the new tablet form might feel like a minor miracle.
LaverdiaAccording to the Veterinary Cancer Society, one in four dogs will develop cancer, and one of the most common types of cancer is lymphoma, caused by malignant lymphocytes (a type of white blood cell). Some breeds (boxers, golden retrievers, Bernese mountain dogs, basset hounds, rottweilers, Saint Bernards, bulldogs, doberman pinchers) are especially prone to lymphoma.
Treatment can include a variety of injectable chemotherapy drugs. Oral prednisone can be of benefit, but typically provides only a short duration of remission. Just this month, the FDA granted full approval for Laverdia, the first oral chemotherapy treatment for lymphoma.
Although Laverdia has lower response rates and shorter remissions than injectable chemotherapy drugs, it’s a valuable, quality‑of‑life–focused option for those who opt out of more aggressive treatment.
Might your dog benefit from potassium bromide tablets or Laverdia? Any interest in enrolling your dog in the TRIAD trial or any other aspect of the Dog Aging Project? As the project states, “We welcome ALL dogs—young and old, large and small, mixed breed and purebred, healthy and those with chronic illness—from all fifty US states. The only requirement is that you have a good estimate of your dog’s age.”
Best wishes to you and your four-legged family members for abundant good health,
Dr. Nancy
DrNancyKay.com
Speaking for Spot - Dr. Nancy Kay is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
January 19, 2026
Preparing for the Unthinkable
It’s hard to imagine our pets outliving us. Worse yet is thinking about how uncomfortable they may feel in a new home while grieving the loss of their favorite human.
 Photo by Jon Tyson on Unsplash
Photo by Jon Tyson on UnsplashAs difficult as it is to consider this possibility, I encourage you to prepare for it in a way that will protect your pets.
Speaking for Spot - Dr. Nancy Kay is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
Just as you are encouraged to create paperwork that makes it undeniably clear who will inherit your possessions and assume guardianship of your children, so too should you specify in writing who will take care of your pets.
Things to considerSelect the person(s) you want to either assume guardianship or be responsible for assigning guardianship. Confirm their agreement and be as specific as possible about the quality of care you would expect.
Once a year or so, check in with your intended guardian to confirm their commitment. You can also fill them in on how your pet’s needs may have changed.
Set up a plan that will provide financially for your pets for the remainder of their lives. Most laws view animals as property. This means they can’t directly inherit money or assets.
Pet TrustsEven if you’re a younger person (cause ya never know), I encourage you to set up a pet trust, a legal document that specifies who will take your pets how you want them cared for when you’re gone. The trust will take effect should you become incapacitated or in the event of your death. (Sorry, I know this stuff is hard to think about.)
A trust is a legally binding document that can include specific care instructions (diet, exercise, medical care, end-of-life decision making, etc.). It can also specify allocation of money for your pets once you can no longer care for them.
Pet trusts exist in every state within the United States. You can find DIY pet trust templates on line, but their validity may vary from state to state. Consider enlisting help from an attorney.
Just think of the peace of mind you’ll have once you get this done!
How have you planned for your pets’ future should you no longer be able to care for them?
Best wishes to you and your four-legged family members for abundant good health,
Dr. Nancy
drnancykay.com
Speaking for Spot - Dr. Nancy Kay is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
January 12, 2026
Urinary Accidents
If your wonderful dog, who has always done his “business” outside, begins leaving puddles in the house, please do not default to the assumption that this is a behavioral issue.

Resist the temptation to think that your dog did this as payback for going somewhere without him or paying too much attention to the neighbor’s dog. Regardless of what they may be feeling, well house-trained dogs would rather urinate anywhere other than inside their own home.
Speaking for Spot - Dr. Nancy Kay is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
The most likely cause of urinary accidents (inappropriate urination) is an underlying medical issue such as the following:
Bladder infections, stones, and tumors create an urgency to urinate even when the bladder contains only a small amount of urine.
Prostate gland diseases can disrupt normal urinary habits.
Increased water intake may overwhelm a dog’s normal eight to ten-hour bladder capacity. Common causes of increased thirst include hormonal imbalances (diabetes, Cushing’s disease, Addison’s disease), kidney failure, and liver disease.
Commonly prescribed medications such as prednisone (a form of cortisone) and furosemide (a diuretic or “water pill”) typically cause increased thirst, leading to increased urination.
Urinary incontinenceUrinary incontinence (involuntary urine leakage) occurs most commonly in female dogs and can be caused by a variety of underlying medical issues.
The urine leakage may be constant, or only occur during the night when the bladder distends in a sound asleep dog who then wakes up in a puddle of urine.
Fixing the problemIn most cases, correcting the underlying medical issue will fix the inappropriate urination and restore your dog’s house training.
If your dog has a break in house-training, please don’t respond with a reprimand. Far better to schedule a consultation with your veterinarian. After all, isn’t this what your beloved dog deserves?
Has your well house-trained dog ever urinated in the house? Were you able to determine the underlying cause?
Best wishes to you and your four-legged family members for abundant good health,
Dr. Nancy
DrNancyKay.com
Speaking for Spot - Dr. Nancy Kay is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
January 5, 2026
Do Dogs Dream?
Scout closes her eyes, and within minutes, her lips are twitching, Then all four legs paddle as if she’s chasing a rabbit, romping in the woods, or running toward home. Whatever’s happening, I hope it’s an amazing dream.
 Photo by Kyle Mesdag on Unsplash
Photo by Kyle Mesdag on UnsplashHappy New Year! For my first post of 2026, I pose the question, do dogs dream?
Speaking for Spot - Dr. Nancy Kay is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
I bet most of us would say, “Of course they do!” Anyone who’s observed a sleeping dog’s vocalizations, wagging tail, paddling feet, and twitching muzzle would likely agree. But the fact of the matter is, we don’t know with scientific certainty that dogs dream.
What we know about dogs and dreamingWhile our knowledge is limited, the following known information supports the notion that dogs do dream.
Matthew Wilson from MIT and Kenway Louie from NYU teamed up to study the relationship of memory, sleep, and dreams in rats. They documented that, when rats are trained to run along a circular track for food rewards, their brains create a distinctive firing pattern of brain cells. The researchers conducted the same brain monitoring while the rats were sleeping. Low and behold, the sleeping rats’ brains had the same signature brain activity pattern associated with running on the track. In fact, the memories played at approximately the same speed during sleep as when the rats were awake. Can we take the information from this study and apply it to dogs? Wilson believes we can because the hippocampus, the portion of the brain that collects and stores memories, is wired much the same way in all mammals. “My guess is — unless there is something special about rats and humans — that cats and dogs are doing exactly the same thing.”
In people, most dreams occur during REM (rapid eye movement) sleep. Dogs also experience REM sleep during which their breathing becomes irregular and shallow. There may be muscle twitching during REM and, when one looks closely, rapid eye movements behind closed eyelids are often observed. It is during REM sleep that behaviors thought to be associated with dreaming (legs paddling, twitching, vocalizing, etc.) are most commonly observed. This matches how humans physically “act out” dreams (minus the barking and tail wagging, of course).
Dr. Deirdre Barrett, a psychologist and dream researcher at Harvard Medical School, thinks it’s safe to assume that dogs dream very much the same way we do. “Whatever you can observe dogs being interested in by day is what you would expect to show up in their dreams. Since most dogs are extremely attached to their human owners, it’s likely your dog is dreaming of your face, your smell and of pleasing or annoying you.”
Sigmund Freud theorized that dreaming is a “safety valve” for our unconscious desires. Perhaps he is correct, and, when our dogs sleep, they dream about finally catching those pesky squirrels or stealing the Thanksgiving turkey off the dining room table.
Do you think your dog dreams? If so, what do you think they’re dreaming about?
Wishing you and your four-legged family members a happy and healthy new year,
Dr. Nancy
DrNancyKay.com
Speaking for Spot - Dr. Nancy Kay is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
December 29, 2025
Capping Off 2025 With a Feel-Good Story
Cali, a 5-year-old pit bull mix, was pregnant when she arrived at Wags & Walks, an animal nonprofit organization. Her 11 pups were quickly adopted, but not Cali. She waited, and waited, and then waited some more.
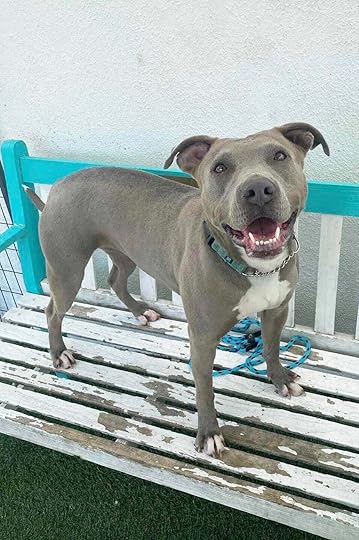 Cali (photo by Wags & Walks)
Cali (photo by Wags & Walks)According to the folks at Wags & Walks, “Cali struggled to feel comfortable around new people. This made finding a home for her a little more difficult.”
Speaking for Spot - Dr. Nancy Kay is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
In a recent Instagram post (be sure to watch this sweet video), Wags & Walks staff described Cali this way:
While Cali was in our care, she became a staff favorite amongst our entire team. She would greet our animal caretakers in her kennel with full-body wiggles, often offering them whatever toys or treats she had as gifts. However, it was difficult for potential adopters to see the sweet and loving girl we all knew her to be.
It took over two years, 798 days to be exact, for someone to finally say, “Cali’s the one.” That someone was Crystal, who lost her dog a few months prior. She sawCali online, visited her, and discovered an immediate connection. Cali is off to a good start in her new home, and Crystal feels certain that love and patience will go a long way with her new best friend.
 Cali (photo by Wags & Walks)
Cali (photo by Wags & Walks)Sigh…I love this happy ending and hope you do too. Do you have a feel-good story to share?
Best wishes for the new year,
Dr. Nancy
drnancykay.com
Speaking for Spot - Dr. Nancy Kay is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
December 22, 2025
My 2025 Reading Recommendations
I tend to gravitate towards things written about animal welfare. Here are a few of my 2025 favorites.
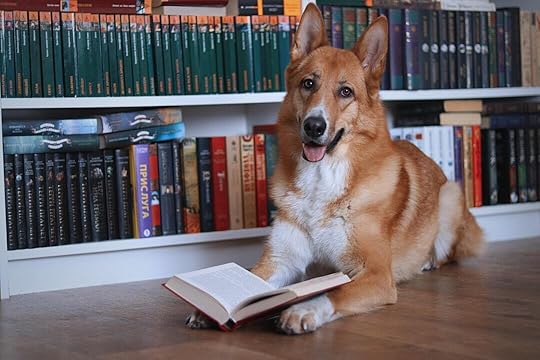 Photo by anotherxlife on UnsplashAnimal Politics With Ed Boks
Photo by anotherxlife on UnsplashAnimal Politics With Ed BoksWith his vast experience in the realm of animal control and sheltering, Ed is an encyclopedia of knowledge about pet overpopulation, specifically what works to diminish it and what doesn’t. His blog posts are passionate, and his interviews with other animal welfare activists always provide insight and inspiration. A recent interview discussing replacement of “no-kill” with “no-birth” was outstanding.
Speaking for Spot - Dr. Nancy Kay is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
Happy DoggoI encourage you to subscribe to his Niall Harbison’s Substack, Happy Doggo. Niall is an Irish superhero who works tirelessly to rescue and care for street dogs in Thailand. His animal welfare organization, Happy Doggo, focuses on feeding and neutering homeless dogs. Through fundraising efforts, he recently constructed a veterinary hospital where sick and injured dogs can be cared for. Niall has a huge global following.
Who Will Let the Dogs OutCara Achterberg must never sleep! Not only is she a blogger, book author, shelter dog advocate, foster dog mom, and human mom, she spends a ton of time on the road gleaning information from her animal shelter visits. Cara is a founder of Who Will Let the Dogs Out, a nonprofit focused on raising awareness and resources for homeless dogs in shelters. Her excellent book, which goes by the same name, highlights shelter challenges with proposed solutions. I encourage you to subscribe to her Substack which addresses pet overpopulation through real-world stories.
The Year of TopsyKim Stallwood is a highly regarded lifelong animal welfare advocate. He’s currently working on a biography of Topsy, an elephant forced into the cruel life of circus animals. You can learn about this in his recent blog post, The Year of Topsy. I’m eager to read the biography and, when I do, I’ll have my Kleenex box handy.
Dog WiseKaren Baril’s writing is beautiful and insightful. Her recent Dog Wise blog post, Ten Ways to Support Homeless Pets This Holiday…even if you’re broke was outstanding. So many terrific ideas here.
Nicholas KristofI was so moved by Nicholas Kristof’s powerful New York Times opinion piece, Animals That Feel the Slice of the Knife. He ends his article with, “What I keep thinking is this: If you torture one animal, you’re arrested and considered a psychopath. But if you abuse millions of animals in a systematic, industrial process, you’re hailed for your business acumen. That’s an uncomfortable contradiction at the heart of modern dining.”
What inspired you in 2025? I’d love for you to share your reading recommendations with me.
Best wishes to you and your four-legged family members for a happy and healthy holiday season,
Dr. Nancy
drnancykay.com
Speaking for Spot - Dr. Nancy Kay is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.



