Options for Postsurgical Pain Management
Whether you’ve been living relatively pain free or dealing with chronic pain for a long time, worry about how you’ll cope with pain after a planned surgical procedure is common. Understanding the benefits and risks of various options and having a plan for pain management helps reduce stress and improve outcome.
This article will review different approaches to postsurgical pain management, starting with different patients’ experiences, then discussing what the research says about different medication options, including a newer, nonopioid medication called Exparel.
A friend of mine I’ll call Paul was admitted to the hospital recently for surgery for suspected lung cancer. Fortunately, the tumor was benign, but the surgery was extensive. It involved a deep incision in his chest, spreading his ribs and removing a portion of his lung. He anticipated being in the hospital for a few days after the procedure but there were no beds available, so he was discharged home less than 24 hours after the procedure with no home care plan in place. When he expressed concern to his surgeon, he was told they weren’t running a hotel. Paul is 75 years old and lives alone.
I spoke with Paul a few days after the surgery and offered to stop by with some of my non-pharmaceutical pain management tools. Paul told me that he was doing okay with pain management. The hospital had sent him home with opioids, but he didn’t want to take them. Instead, he had been managing his pain with Tylenol. He said the first day getting in and out of bed was excruciating but it had been improving every day and he wasn’t feeling the need to use anything but Tylenol.
Paul is a courageous sort. He frequently travels solo and low budget to India, Thailand, Cambodia, Mexico and other countries that can be hazardous. He has had some harrowing adventures but continues to go back to those countries again and again.
I’m much more of a wuss than Paul. I’m not fond of physical risks and, having had more than my share of pain in my lifetime, I didn’t want to deal with it any more than I had to. A few years ago, I was accidentally tripped by a department store employee and broke my right ankle. I needed surgery because the bone was displaced. The surgery involved a long incision in my leg and placement of a plate and screws. Like Paul, I didn’t want to use opioids. For years, I had been developing expertise in nonpharmaceutical pain management for personal and professional use and educating others about it. I had many tools on hand. I thought, “Nobody is better prepared than me to address acute pain management without opioids” and I decided to practice what I preach.

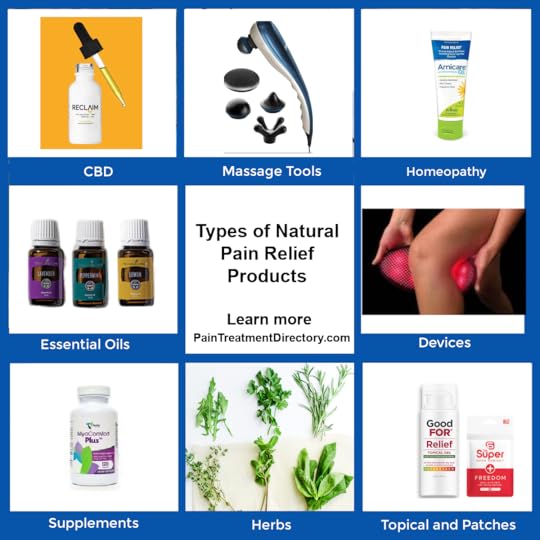
I used CBD and medical marijuana gummies, homeopathic remedies, low level laser therapy, pulsed electromagnetic frequency (PEMF) therapy and, on occasion, a dose or two of ibuprofen. Also, a client introduced me to kratom, a southeast Asian herb that I found to be the most powerful pain reliever of all. I managed to stay fairly comfortable throughout my recovery.
Charlena, my website marketing manager, gave birth by planned ceasarian section to her daughter three years ago. Then, just a few months later, she had surgery for a benign brain tumor. Both times, Charlena assured me she'd be right back to work afterwards. I didn't really believe her, but she was! More remarkably, beyond whatever pain meds she was given during her short hospital stays, she didn't use anything for pain. She said she didn't have any real discomfort.
As you can probably tell, Charlena has a real can do attitude and doesn't let much of anything get her down.
Most patients expect to receive opioids for post operative pain control. They have been hearing for decades that the best thing we have for pain is opioids and they become angry and bitter when they are denied opioids postsurgically or are only given a few days’ supply. They expect to have inadequate postoperative pain control without opioids, and that expectation can have a powerful effect on their subsequent pain levels.
Find an Alternative Pain Relief Provider
Safety and Effectiveness of Other Pharmaceutical Options
Exparel: A newer, nonopioid drug for postsurgical pain management
Due to concerns about opioid addiction, pharmaceutical company Pacira Biosciences developed Exparel for postsurgical pain management. Exparel is a long-acting local anesthetic. Its active ingredient is bupivacaine, packaged in tiny fat-like “liposomes” designed to release medication slowly. It is meant to numb tissues or nerves for longer than standard bupivacaine, so you have less pain during the first couple of days after surgery.
Exparel is not a pill you take at home. It is given during surgery by your surgeon or anesthesiologist in one of two main ways:
Local infiltration: injected into the tissues around the surgical site (this can be used in patients aged 6+).Specific nerve blocks in adults (regional analgesia):Interscalene brachial plexus block (often for shoulder surgeries)Sciatic nerve block in the popliteal fossa (often for foot/ankle procedures)Adductor canal block (often for knee procedures)
How effective is Exparel?
Exparel can Lower pain scores during the first 24–72 hours, and/or result in less opioid use after surgery (opioid-sparing effect)
For example, a meta-analysis in breast procedures found reduced postoperative opioid consumption when liposomal bupivacaine was used in certain breast surgeries, though results differed depending on the specific procedure (benefit was clearer in reconstruction and aesthetic procedures than mastectomy without reconstruction).
There are also trials showing Exparel can be about as effective as standard approaches and may reduce opioid use in certain settings, but not consistently across the board.
Bottom line on effectiveness
Best-case scenario: It meaningfully reduces pain for the first couple of days and helps you need fewer opioids.Common scenario: It helps somewhat, but you still need a full multimodal plan.Sometimes: It does not outperform simpler, less expensive options (especially depending on the procedure and how pain is managed overall).
Side effects and risks of Exparel
Because Exparel is a local anesthetic, many people tolerate it well, but it still has real risks.
Common side effects reported in clinical studies: nausea, constipation, vomiting, headache, and fever, depending on whether it is used by infiltration or nerve block.
Serious risks (less common)
Local anesthetic systemic toxicity (LAST): If local anesthetic levels get too high (or if accidentally injected into a blood vessel), it can cause dangerous neurologic or heart effects. The label notes seizures and cardiac arrest have occurred with accidental intravascular injection of bupivacaine products.Numbness/weakness and falls/injury risk: Nerve blocks can leave a limb numb or weak, so you may not protect it normally.Drug interaction timing: You generally want to avoid additional local anesthetics within 96 hours after Exparel because blood levels can persist.What the research says about other drugs for postsurgical pain management
Evidence has been accumulating for years that using ibuprofen and/or acetaminophen (Tylenol) works just as well or better than opioids for postoperative pain control with fewer side effects and risks. A study of more than 22,000 patients at 70 hospitals by the University of Michigan and published in 2021 in Annals of Surgery found that patients treated with ibuprofen or acetaminophen didn’t have higher pain levels or lower satisfaction with their care than patients treated with opioids. Those who didn’t receive opioid prescriptions were more likely to report no pain in the first week after surgery than those who did (12% vs 7%). The non-opioid patients were also slightly more likely to say they had the best possible quality of life after surgery (66% vs 63%).
A randomized double-blinded study of pain management after carpal tunnel release surgery published in 2018 in the Journal of Hand Surgery compared Oxycontin, ibuprofen and acetaminophen. The nonopioid medications outperformed Oxycontin for pain relief. The average worst daily pain scores for all days for the Oxycontin, ibuprofen, and acetaminophen groups were 3.4, 2.5, and 2.3, respectively. Four of 5 adverse events were reported by Oxycontin group patients, though all were minor.
A study conducted at Magill University Health Center and published in The Lancet in 2022 concluded that prescribing opioids at discharge after surgery does not reduce postoperative pain compared to non opioid medications and increases the risk of adverse events. The study included the results of 47 randomized clinical trials of minor and moderate extent surgical procedures. According to principal investigator Julio Fiore Jr., PhD, “We found that prescribing opioids had no impact on patient-reported postoperative pain control compared to simple over-the-counter analgesics, but it significantly increased the risk of adverse events, such as nausea, vomiting, constipation, dizziness and drowsiness.” He added, “Prescribing non opioid medications may prevent these adverse effects, improve patients’ recovery experience, and also help mitigate the opioid crisis by reducing the risk of postoperative opioid misuse, addiction and diversion.” He also reported that approximately 6% of surgical patients who’ve never used opioids before become persistent opioid users after receiving a prescription post surgically. This percentage was also reported in a study published in 2017 in JAMA Surgery, which found no difference whether the surgical procedure was major or minor.
“Opioid analgesics are not widely used in the postoperative setting in Europe, Asia, the Middle East and South America. The reasons contributing to the widespread use of postoperative opioids in North America are multifactorial but include clinicians’ concerns regarding inadequate pain control, patient dissatisfaction and risk of increased emergency visits due to uncontrolled pain,” explains Charbel El-Kefraoui, co-first author of the study. “Findings from our study indicate that none of these concerns are supported by evidence.”
There are a few cautions about using ibuprofen postsurgically, including delayed healing. Here's a list of possible issues with postsurgical pain management with ibuprofen:
Inflammation Reduction: Ibuprofen works by inhibiting the production of certain chemicals (prostaglandins) that cause inflammation and pain. In the context of surgery, some level of inflammation is a natural part of the body's healing response. In some cases, a controlled amount of inflammation can be beneficial for tissue repair. Using ibuprofen immediately after surgery might potentially interfere with this initial healing process.Impaired Bone Healing: Some studies have suggested that NSAIDs like ibuprofen could potentially hinder bone healing, which could be a concern for surgeries involving bones. The exact impact might depend on the dosage, timing, and duration of ibuprofen use.Gastrointestinal Concerns: NSAIDs are known to increase the risk of gastrointestinal bleeding and ulcers, which could be particularly concerning after surgery when the body is already under stress.Renal Function: NSAIDs can affect kidney function, and this could be relevant for patients who are at risk of kidney issues or who have undergone surgeries that could impact renal function.Bleeding Risk: There's also a potential concern about NSAIDs increasing the risk of bleeding, especially for surgeries where bleeding could be an issue.
There are also indications that opioids negatively affect postsurgical healing, including:
Suppressed Immune Function: Opioids can suppress the immune system, making it less effective at fighting off infections. This can potentially lead to an increased risk of postoperative infections.Delayed Wound Healing: Opioids can affect wound healing by reducing blood flow to the surgical site. Proper blood flow is crucial for delivering oxygen and nutrients to the tissues, which aids in the healing process. Reduced blood flow can lead to delayed wound healing and increased risk of complications.Constipation: Opioids are known to cause constipation, which can be a significant concern after surgery. Straining during bowel movements can put stress on surgical incisions and disrupt the healing process.Respiratory Depression: High doses of opioids can cause respiratory depression, where breathing becomes slow and shallow. This can potentially lead to decreased oxygen supply to tissues, which is essential for proper healing. Severe respiratory depression is what causes opioid overdose deaths.Mobility and Physical Therapy: Pain is a natural indicator that helps regulate movement. If pain is too effectively managed with opioids, patients might overexert themselves and potentially cause damage to surgical sites. Additionally, reduced pain perception might discourage patients from engaging in necessary physical therapy, which can slow down recovery.Psychological Effects: Opioids can impact mood, cognitive function, and overall mental state. These effects might influence a patient's motivation to engage in healthy behaviors, follow postoperative care instructions, and maintain a positive outlook on recovery.
And I probably could have simplified my own postoperative pain regimen.
Please note that both ibuprofen and acetaminophen can be dangerous with chronic use so it's important to find other options for chronic pain relief.
The author, Cindy Perlin, is a Licensed Clinical Social Worker, certified biofeedback practitioner and chronic pain survivor. She is the founder and CEO of the Alternative Pain Treatment Directory and the author of T he Truth About Chronic Pain Treatments: The Best and Worst Strategies for Becoming Pain Free . She's located in the Albany, NY area, where she has been helping people improve their health and emotional well-being for over 30 years. See her provider profile HERE . She is available for both in-office and virtual consultations.
Related Articles:
Kratom as an opioid Alternative
Marijuana as an Opioid Alternative
The Opioid Crisis and what we can do about it